Pain Relief Research: Clearing the Smoke Surrounding Cannabis
Members of the Comprehensive Center for Pain and Addiction are optimistic about the potential of cannabis as a viable non-opioid alternative to treat pain.

Researchers in the Comprehensive Pain and Addiction Center are studying cannabis with a focus on pain, inflammation and addiction.
Cannabis. It’s a word surrounded by controversy. In the United States, public opinion and politicians have long grappled with the legal, ethical and societal implications of its use. What regulations are needed? Is it addictive? Is it safe? Only recently have scientists begun to unravel the mysteries of Cannabis sativa, a plant that is cultivated for food, fiber and, in every part of the world, medicinal use.
At the University of Arizona Health Sciences, researchers are expanding the scientific knowledge of cannabis with a focus on two distinct areas – pain and addiction. Leading the way is Todd Vanderah, PhD, interim director of the UArizona Health Sciences Comprehensive Center for Pain and Addiction. Dr. Vanderah has spent two decades studying cannabinoids – the compounds found in cannabis.
Todd Vanderah, PhD, director of the Comprehensive Center for Pain and Addiction, has been studying cannabinoids for nearly two decades.
“I've worked at seeking to understand chronic pain for many years, trying to figure out how we could develop new compounds to help people with pain that weren't opiates and weren't addictive. One of the areas we began to explore was cannabinoids,” said Dr. Vanderah, a professor and chair of the Department of Pharmacology in the UArizona College of Medicine – Tucson and member of the BIO5 Institute.
Cannabis contains more than 500 chemical compounds. THC, or tetrahydrocannabinol, is the cannabinoid responsible for the plant’s psychoactive effects and as such, has been the focus of much research through the years. CBD, or cannabidiol, has a chemical structure slightly different than THC and doesn’t produce psychoactive effects, yet there is little known about the activity of CBD.
Much less is known about other cannabinoids or other parts of the plant, such as terpenes, which give cannabis its distinctive aroma and taste.
“We are only just beginning to understand all of the different chemicals that are naturally present in cannabis,” Dr. Vanderah said. “I'm probably the most excited about understanding the endocannabinoid system.”
Those are the cannabinoids that the human body makes.
Identifying naturally occurring cannabinoids
Most people know endorphins cause the “runner’s high” often experienced by athletes. Endorphins are the body’s endogenous, or naturally occurring, opioids. Once produced, endogenous opioids activate receptors that produce physiological changes such as pain relief.
Medical marijuana is currently legal in 36 states, though it remains illegal at the federal level. The classification of cannabis as a Schedule I drug has made it challenging for researchers to study.
Exogenous opioids, those that are not naturally produced and originate from outside the body, work by co-opting the endogenous opioid system. Prescription drugs such as oxycontin target and activate opioid receptors. Once activated, the receptors produce the same result as endorphins: pain relief.
In a similar fashion, the body produces endogenous cannabinoids. While scientists have been studying the endogenous opioid system since the 1970s, research into the endogenous cannabinoid system, or endocannabinoid system, is still in its infancy. Researchers know endocannabinoids play a role in maintaining cellular balance, and many believe the endocannabinoid system also helps regulate functions such as mood, appetite and sleep.
“Our bodies make cannabinoids, and we make plenty of them,” said Dr. Vanderah, who began studying cannabinoids in the early 2000s. “A number of studies have shown that physical exercise increases the amount of endocannabinoids in circulation, just like endorphins. One review pointed out that stress can release endocannabinoids, and the increased levels of endocannabinoids may actually decrease some of that stress.”
“We are only just beginning to understand all of the different chemicals that are naturally present in cannabis.”Todd Vanderah, PhD
Early cannabinoid research has identified two cannabinoid receptors and enzymes that make and break down endocannabinoids. The receptors, dubbed CB1 and CB2, are located throughout the body, including in the central and peripheral nervous system.
“CB1 is interesting in that some people suggest it's the highest concentrated receptor in the human brain, and we know that compounds that act at the CB1 receptor will produce psychotropic effects,” said Dr. Vanderah, who has directed much of his research at the lesser-studied CB2 receptor. “CB2 receptors are found more on immune cells, and they tend to be on the immune cells of the bones, spleen, colon, liver and pancreas.
“We know there are CB1 and CB2 receptors functioning in many parts of the body. For example, we know there are a lot of receptors in the lungs,” Dr. Vanderah added, “but we don't know what they are doing there. There is a lot of research that needs to be done.”
With many of the internal mechanisms of the endocannabinoid system identified, researchers are seeking to understand how specific cannabinoids act on those mechanisms, whether changes in the endocannabinoids are related to disease states, and how the endocannabinoid system can be modulated to develop new treatments for pain and inflammation.
To that end, much of the current endocannabinoid research focuses on two areas: substances that may act as CB1 and CB2 agonists, meaning they activate the receptors; and enzyme modulators that would alter levels of endocannabinoids.
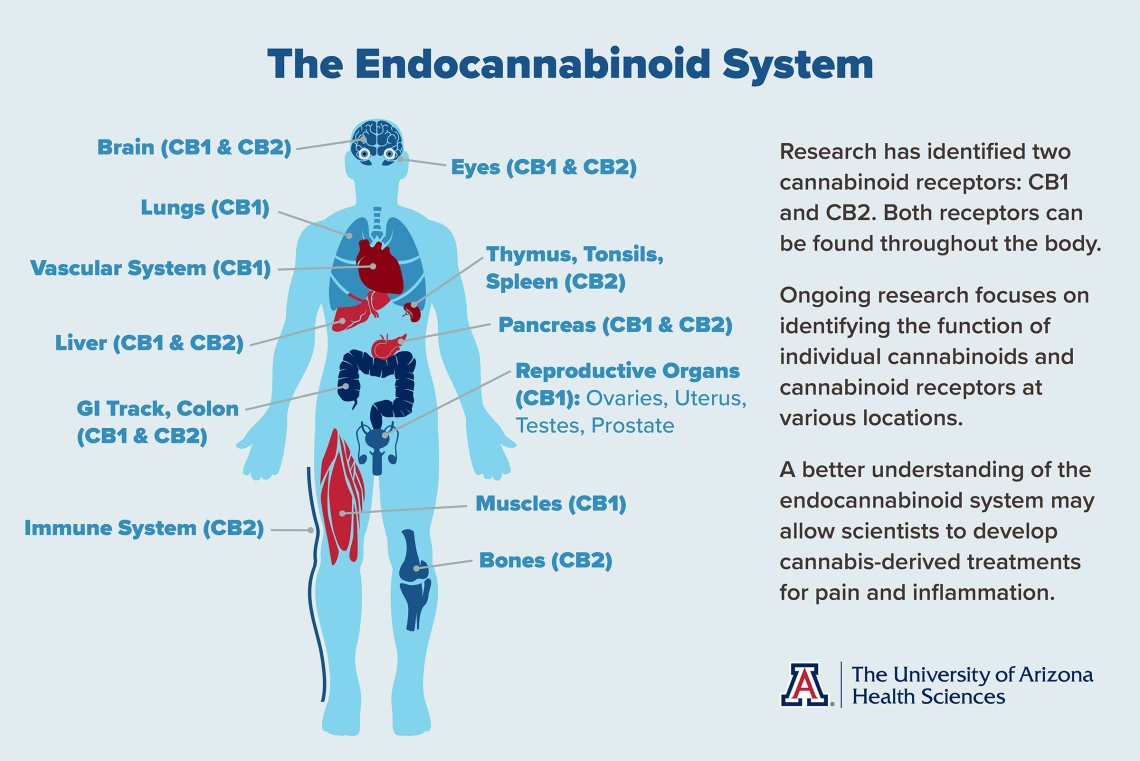
Click to enlarge.
Finding answers through science
Researchers in the Comprehensive Pain and Addiction Center are examining cannabinoids on several different fronts, many of them with a focus on different kinds of pain including chronic, neuropathic and cancer-related.
Tally Largent-Milnes, PhD, assistant professor in the College of Medicine – Tucson and a member of the BIO5 Institute, focuses on migraine pain in her laboratory in the Department of Pharmacology. One of the questions she hopes to answer is whether a decrease in endogenous cannabinoids correlates to an increase in migraine headaches. Understanding how the endocannabinoid system regulates pain in headache disorders could lay the foundation for a pathway to novel migraine therapeutics.
John Streicher, PhD, an associate professor of pharmacology in the College of Medicine – Tucson, is examining terpenes, the part of the cannabis plant that provides flavor and aroma. A recently concluded study showed that terpenes, when used by themselves, mimic the effects of cannabinoids, including a reduction in pain sensation. When combined with cannabinoids, the pain-relieving effects were amplified without an increase in negative side effects.

As cannabis becomes more readily available throughout the U.S., researchers are using science to separate fact from fiction as they unlock the secrets of the endocannabinoid system. (Credit: My 420 Tours, CC BY-SA 4.0, via Wikimedia Commons)
Dr. Streicher’s ongoing research is focusing on the use of terpenes in combination with opioids and for specific types of cancer-related pain. His long-term goal is to develop a dose-reduction strategy that uses terpenes – generally recognized as safe by the U.S. Food and Drug Administration – in combination with cannabinoids or opioids to achieve the same levels of pain relief with lower doses of drugs and fewer side effects.
Pavani Chalasani, MD, MPH, an oncologist, associate professor in the College of Medicine – Tucson and UArizona Cancer Center member, and Dr. Vanderah collaborated on a recently concluded clinical trial that studied the effects of dronabinol, a pharmaceutical form of THC, on metastatic cancer pain. The results of that trial should be available later this year. Dronabinol, one of two cannabinoid products approved by the FDA, is prescribed to treat nausea and vomiting caused by chemotherapy.
Outside of dronabinol, the federal government considers cannabis a Schedule I drug, which makes research challenging. Cannabis use remains federally illegal, as it has been in the U.S. since 1937, though 38 states allow for the use of medical marijuana and 21 allow for recreational use of cannabis.
“It's unfortunate that the whole general population of cannabinoids falls under this biased idea people have about medical and recreational marijuana, because you can't lump it all together,” Dr. Vanderah said. “It's a big family of chemical structures that we just don't know enough about yet. The best thing is there are more studies being done in this field, and we’re learning a lot, day by day. Nature has made a lot of useful plants, from aspirin to chemotherapeutics to antibiotics, and there are things in cannabis that could be medicinally beneficial.”
Researchers in the Comprehensive Center for Pain and Addiction are examining cannabinoids from several different fronts, many of them with a focus on different kinds of pain and inflammation.
Contact
Stacy Pigott
520-539-4152
spigott@arizona.edu

