Mechanical Devices as Small as Cell Phones Buy Quality Time for Patients with Advanced Heart Disease
When it comes to mechanical heart devices, downsizing has been a good thing.
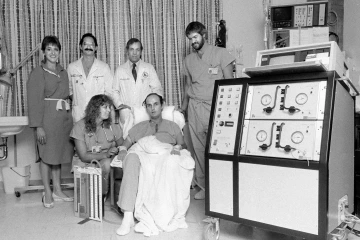
In 1985 when the University of Arizona heart transplant program implanted the artificial heart as a bridge to heart transplant, patient Michael Drummond was tethered to “Big Blue,” a power driver that required him to remain hospitalized until a donor heart was found. He received a donor heart nine days later and was the world’s first successful “bridge-to-transplant” patient.
In 1985, when the University of Arizona and then-University Medical Center were making history as the first medical center to successfully use a total artificial heart as a bridge to heart transplantation, “Big Blue,” the size of a washing machine, powered the device.
Total artificial heart patients were tethered to Big Blue and hospitalized until a donor heart became available for transplant – which sometimes took more than a year.
Today patients at Banner – University Medical Center Tucson still receive total artificial hearts, but instead of remaining in the hospital, they enjoy life at home participating in normal activities. The modern version of Big Blue fits in a backpack.

Jennifer Cook, MD, medical director of the Advanced Heart Failure, Mechanical Circulatory Support and Cardiac Transplantation Program, holds a heart-assist device and power source in front of the ever-evolving display of devices available to buy quality time for heart-failure patients.
Further, implantable monitoring devices also improve quality-of-life for advanced heart disease patient care.
For example, patients, like Deborah Martinez, now have access to an implantable monitoring system called CardioMEMs that measures blood pressure in the lungs. The entire device is about 4 inches wide – two wires that form a loop around a chip – and is implanted through the veins. From their home, patients can record heart pressure measurements by simply lying down on a pillow for 17 seconds. The information is sent electronically and can be viewed by their doctor online.

Angelica Lentner, NP, explains data captured by CardioMEMS to patient Deborah Martinez, her husband, Frank, and son, Francisco.
In a recent CardioMEMS clinical trial, the device reduced hospital admissions by 37 percent.
Technology for advanced heart disease is a growing field, considering the enormity of heart failure in the United States. About 6.5 million people are living with heart failure, a number projected to rise 46 percent to 8 million patients by 2030. The cost of care is estimated to be more than $10 billion per year in the United States alone.

Typical heart failure symptoms include difficulty breathing, walking and participating in normal activities.
Heart Failure Awareness Week concludes Feb. 17. The Heart Failure Society of America encourages individuals to “Do Your Part. Know Your Heart.” Visit UA Sarver Heart Center’s Advanced Heart Disease web section to learn more.
We encourage everyone to talk with your loved ones about their organ donation wishes and complete a donation registration form. Also, please complete a Cardiology Research Registry Information Form to learn about new clinical research studies for which you may be eligible.
About the Author
Jennifer L. Cook, MD, is an associate professor of medicine at the University of Arizona Sarver Heart Center and director of Advanced Heart Failure, Mechanical Circulatory Support and Cardiac Transplantation at Banner – University Medical Center Tucson.

