Reframing Public Health Crisis Resilience
On the cusp of a new role to reduce statewide COVID-19 disparities, Dr. Mona Arora discusses public health preparedness, climate change and the pandemic.

Dr. Mona Arora, an assistant professor of public health, co-chaired the UArizona Vaccine Task Force. Her newest role is co-leading a statewide effort to improve vaccine rates and address related health disparities that’s funded by the CDC and Arizona Department of Health Services.
Finding the good in the world during a pandemic can come from simple things such as baking cookies with a child, nature walks or completing a jigsaw puzzle.
Mona Arora, PhD, MSPH, makes sure she schedules these moments into her life as often as possible, as her position at the University of Arizona Health Sciences requires her to be involved in a complicated, long-range blending of public health and the impact of climate change.

Dr. Mona Arora (center) with Chris Kopach (left), head of the UArizona COVID-19 Incident Command Team and her co-chair of the university’s vaccine task force, give instructions to volunteers at the start of a shift for the UArizona point-of-distribution (POD) clinic. (Courtesy Mona Arora, PhD, MSPH)
A Tucson native who received her bachelor’s degree at UArizona, Dr. Arora earned her Master of Science in Public Health from Tulane University School of Public Health and Tropical Medicine in New Orleans. Her first semester there in 2004, she evacuated to Houston during Hurricane Ivan. While in India to do her master’s thesis on vector borne diseases, Hurricane Katrina struck New Orleans and she couldn’t go back to Tulane. So she came home to Tucson.
“If you're working in tropical medicine, you're working on infectious diseases, the desert is not the place you want to be,” she admitted. “But I was thinking about my experience from Hurricanes Ivan and Katrina, and what emergencies would happen here that would necessitate emergency planning.”
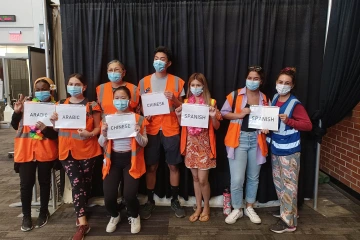
Volunteer interpreters on the final week of vaccine administration for the UArizona point-of-distribution (POD) clinic in June. (Courtesy Mona Arora, PhD, MSPH)
In many ways, public health planning for climate- and pandemic-related crises is the same, Dr. Arora said. “Whether it’s heat emergencies, extended fire seasons, severe weather, stronger and more frequent hurricanes or global events like COVID-19, it’s all about building and reinforcing systems and networks that are resilient and adaptable,” she said. “Those systems and networks also need to be equitable to minimize fallout that disproportionately impacts rural and disadvantaged communities. COVID-19 taught us that.”.
Her earlier work prepared her for her current role as co-chair of the University of Arizona COVID-19 Vaccine Task Force. She oversaw the administration of nearly 250,000 vaccines at the Point of Distribution (POD) clinic on the UArizona campus this year.
Taking efforts statewide
Now, Dr. Arora will co-lead an Arizona Center for Rural Health (CRH) statewide outreach program funded by the Centers for Disease Control and Prevention’s COVID-19 Disparities Initiative in collaboration with the Arizona Department of Health Services (ADHS). The initiative aims to reduce COVID-19 disparities, provide vaccinations and promote vaccine confidence in high-risk, rural and underserved communities.

Arizona Department of Emergency and Military Affairs Director Major General Michael T. McGuire consults with Dr. Arora at the walk-in vaccine clinic in the Ina E. Gittings Building just off the UArizona Mall. (Courtesy Mona Arora, PhD, MSPH)
Daniel Derksen, MD, UArizona Health Sciences associate vice president for health equity, outreach and interprofessional activities, and director of the Arizona Center for Rural Health serves as principal investigator on the CDC-ADHS funded project, with Dr. Arora as co-leader. “We are extremely fortunate to have Dr. Arora on the CDC-ADHS COVID Disparities Initiative leadership team. Her commitment and passion blend perfectly with her expertise to advance health equity building on our Center for Rural Health partnerships across the state,” he said.
Under this grant, the UArizona Center for Rural Health will work with critical access hospitals, rural health clinics, community health centers and community health workers to reduce COVID-19 related disparities. The center will deploy resources through the Area Health Education Center Program and its five AHEC Regional Centers, targeted multimodal messaging using the Arizona Telemedicine Program platform, and county and tribal health departments.
Other tools include the Mobile Outreach Vaccine Education for Underserved Populations (MOVE UP) Program, with mobile health units in urban and rural pockets to improve vaccine rates, and an Advancing Health Equity, Addressing Disparities in Arizona (AHEAD) Program that includes a champions campaign to enlist and train local vaccine advocates. These last two create the initiative’s key areas of focus and its motto: “MOVE UP and AHEAD in Arizona.”
“We need to redouble our efforts in rural communities,” said Dr. Derksen, who underscored vaccine challenges in a recent PBS report. “We could do better than we’re doing right now in these pockets.”
Defining success
“Public health is all about anticipating. You anticipate what's going to happen, and you start preparing. We don't have a magic bullet. There's no one solution to all of this. It's consistent education.”Mona Arora, PhD, MSPH
Success hinges on providing trusted information, assuring ready access to services and overcoming vaccine hesitancy. Dr. Arora considers local champions who will be recruited and trained as critical to the efforts. These champions also will be important in the fall when seasonal flu and COVID-19 will circulate simultaneously, with the opportunity to improve uptake as COVID vaccines receive emergency use authorization for school age children.
“With delta and new variants, we're going to see more challenges coming our way,” she said. “We need to mobilize champions to help us get into those pockets to increase the vaccination rate.”
Dr. Arora is working to reframe the message to better communicate the dangers of COVID-19 and the benefits of vaccination, masking, social distancing and hygiene.
“If people are engaged and we have transparency, we’ll have more ownership of the decisions and programs that are being implemented,” she said of her vision to engage all counties. “That will lead to more successful public health interventions.”
Learning by experience
In 2006, Dr. Arora began her UArizona career as lead curriculum developer and trainer for the CDC-funded Mountain West Preparedness and Emergency Response Learning Center at the UArizona Zuckerman College of Public Health, which works to build community resilience for disasters, partnering with rural and tribal communities and local health departments.
She currently provides climate change counsel to the National Association of City and County Health Officials and is member of the Lancet Countdown, which tracks health impacts of climate change. She earned her PhD from the UArizona School of Geography, Development and Environment in 2019.
Her emergency preparedness work now revolves around her doctoral dissertation, “a needs assessment of public professionals working in a climate or health space,” she said. “We must learn from our COVID-19 response as we prepare to deal with a future of increased and intense disasters.”
A sign of strength
Dr. Arora will draw on her emergency preparedness experience to make a difference in the challenges ahead.
“My overall vision is to not duplicate efforts, but to keep the dialogue going,” she said. This includes bolstering equity and sustainability in the public health system during a crisis.

Dr. Arora with Chris Kopach (left), Campus Health nurse Sara Little, Dr. Arora and POD Staffing Lead, Renee Hernandez celebrate the UArizona POD’s final day of operation, June 25, after nearly 250,000 doses administered since January.
With an ever-changing virus and evolving policies to mitigate its transmission, morbidity and mortality, the ability for science to adapt as new information comes to light isn’t a sign of weakness, she said. It’s a sign of strength.
For herself, Dr. Arora finds strength in her child and youth in general. Leaving a better world for them is what drives her.
“They’re our future, and they have a right to be concerned about the kind of world we are leaving them,” she said.

