Dr. Judith Hunt: Rural Medicine’s Change Agent
A College of Medicine – Tucson alumna shares her experiences as a modern pioneer introducing rural medicine to the next generation of health professionals.

Judith Hunt, MD, has found her home practicing rural medicine in Payson, Arizona.

Dr. Hunt and medical student Jeremy Winkleman make a home visit to check on a patient and her new daughter.
Judith Hunt, MD, always knew she wanted to practice rural medicine. The idea was solidified when she was widowed during her residency; she wanted to provide the stability of the rural upbringing she experienced to her then 3-year-old daughter.
She found that stability in Payson, Arizona, a town of about 15,000 that’s “an hour and a half to anywhere,” she said, on its own “island in the Tonto National Forest” that butts up against the Mogollon Rim in the center of the state.
Home is where the heart is
Dr. Hunt, a 1991 graduate of the University of Arizona College of Medicine – Tucson, did rotations through the Arizona Area Health Education Center program in Nogales, Arizona, under internist George Comerci, Jr., MD.
“I was sure that I was going to be only a pediatrician until I worked with Dr. Comerci,” she said. “The time I spent in Nogales prepared me for being an internal medicine/peds doctor in Payson.”

Dr. Hunt holds Amara Lopez while Winkleman listens to her heart during a home health visit.
Today, she practices at the Ponderosa Family Care Rural Health Clinic and the Payson Christian Clinic, a mercy care clinic she co-founded that provides free care for under- and uninsured patients. She also provides newborn and pediatric care at Banner Payson Medical Center, a local 26-bed critical access hospital. About 60% of her practice is children and 30% women. Her patients range from newborn to 100 years old.
As one of a handful of physicians practicing in the Payson area, Dr. Hunt can’t easily send a patient to a specialist or hospital in Phoenix.
“Our medical community likes each other and knows one another’s gifts. We try to find ways to give that excellent care without patients having to go to the Valley,” she said. “We are a small boat and we all row.
“Our lives aren’t separated by our job versus home. My patients are my neighbors or kids I've coached in swim team. They're people I see at the store and I go to church with,” she said, underscoring a sense of community required of rural doctors. She recalled a medical student who was flustered at seeing a patient in the grocery store. “‘She was getting Rice Krispies,’” the surprised student said to Dr. Hunt.
A team effort
As a physician, Dr. Hunt not only treats a surprisingly diverse range of patients, but also trains students from UArizona Health Sciences colleges and beyond.
“Our lives aren’t separated by our job versus home. My patients are my neighbors or kids I've coached in swim team.”
Judith Hunt, MD
She is the regional site director for the University of Arizona College of Medicine – Phoenix’s Rural Health Longitudinal Integrated Clerkship, which started in 2020. It was created through a partnership of the college’s Rural Health Professions Program and the MHA Foundation to address Arizona’s physician shortage, particularly in rural communities. Third-year medical students can earn a Certificate of Distinction by spending nine months living and training in rural clinical settings.
In addition, she is part of a team that is applying for a rural track for residents.
“As we train medical students for rural, some want to continue their training as rural residents,” Dr. Hunt said. “We hope this allows graduating residents to choose rural medicine with all the tools needed for a different type of medicine. Rural medicine may not have its own boards, but it is a specialty.”
She is a preceptor for rural rotations through the Rural Health Professions Programs (RHPP), run by the Arizona Area Health Education Center. Students from all three state universities can participate in the RHPP.
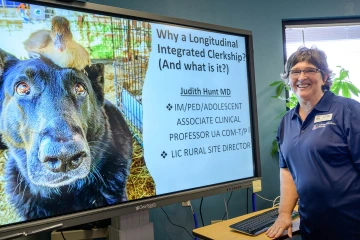
Dr. Hunt is the regional site director for the University of Arizona College of Medicine – Phoenix’s Rural Health Longitudinal Integrated Clerkship, created through a partnership of the college’s Rural Health Professions Program and the MHA Foundation to address Arizona’s physician shortage, particularly in rural communities.
“Our campus is intentionally interprofessional,” Dr. Hunt said. “They're learning together, so they’ll be used to working in a team in a rural area.”
In 2018, Dr. Hunt received the Rural Preceptor Teaching Award from the College of Medicine – Tucson. In mid-July, she was presented with a 2022 Rural Women’s Health Champion Award for her practice’s “Innovative Approach to Rural Women’s Health” at a symposium hosted by the Arizona Rural Women’s Health Network and Arizona Alliance for Community Health Centers.
“This award is really a joint honor because we found out during the pandemic that rural communities are stronger, more courageous and much more creative than we ever thought we could be,” she said in her acceptance speech. “We need to thank COVID for that opportunity to find out who we really are.”
Remote community care
That opportunity came early in the pandemic with the announcement of shelter-in-place orders. Within 24 hours, the entire Payson medical community shifted to telemedicine for most clinical appointments, in part with assistance from medical students on rotation, Dr. Hunt said.
“We’d been doing telemedicine before, so we had those foundations. But the medical students were instrumental in getting that program running so quickly and so effectively. We were all in that same boat learning together,” she said.
Telehealth visits recently expanded due to a Payson Christian Clinic grant supplying “telemed kits,” complete with a blood pressure cuff, pulse oximeter device and electronic stethoscope, to the nearby communities of Tonto Basin, Young, Fo

As a rural physician, Dr. Hunt sees patients ranging from newborns to 100 years old. Here, she speaks with patient Tammy Walp in the clinic.
rest Lakes and Pine-Strawberry. Volunteers take the kits to a person’s home and set them up. The availability of the kits, coupled with not having to drive to appointments, makes it more likely patients won’t miss an appointment, Dr. Hunt said.
Dr. Hunt has first-hand knowledge of the difficulties people in rural areas face when it comes to accessing health care. She grew up near Lake Erie, about 25 miles outside of Buffalo, New York, in the rural town of South Wales, nestled between farmland and a few ski slopes. As a child, heading into the city to get care was like going to another world, she said.
“There was very little appreciation as to what it meant to be a farmer and not be close to a drugstore, not have a clinic nearby. Going to a doctor's appointment took an hour to get there. You were there for 10-15 minutes, and then you went home,” Dr. Hunt said. “There was a big disconnect as to what people's lives were like day-to-day and an unrealistic expectation on patients from the doctor’s perspective.”
She’s working to change that.

