School Asthma Expert Dr. Lynn Gerald Lightens Her Load
A champion powerlifter, this behavioral scientist readies for a sabbatical to study how to promote uptake of asthma research findings into routine practice.

Lynn Gerald, PhD, MSPH, a behavioral scientist at the Mel and Enid Zuckerman College of Public Health, shows a child how to use a stock inhaler to control asthma. She encouraged the Arizona Legislature to pass a 2017 law to improve access to inhalers and broaden who could administer them to students.
Lynn B. Gerald, PhD, MSPH, is used to heavy lifting.
With roles as Distinguished Outreach Faculty and the Zuckerman Family Endowed Chair in Prevention and Lifestyle Medicine at the University of Arizona Mel and Enid Zuckerman College of Public Health, lightening her workload in anticipation for a year-long sabbatical beginning in July has been the opposite of the preparation she needed to become a national record holder as a powerlifter.

A renowned researcher on school policies to promote better asthma care, Lynn Gerald, PhD, MSPH, got into weightlifting as well as aerobics after her undergrad years as a way to stay fit and earn extra cash as a certified trainer.
While powerlifters steadily increase their weight load to get stronger and more comfortable with the additional burden, unloading academic duties is what Dr. Gerald is engaged in now as she prepares to dedicate time to study how to better structure clinical trials and public health research to be more effective.
“I’ve always trained in the early morning before work,” Dr. Gerald said. “I train six days a week for about two hours. When I was doing powerlifting competitions, this focused on the three major lifts – bench, squat and deadlift – with some accessory lifting about five times a week. I also ran and did metabolic conditioning 3-5 times per week, with more focus on weights closer to competitions.”
Dr. Gerald’s dedication to fitness goes beyond powerlifting. She is a certified aerobics, CrossFit and personal trainer. She has even competed as a ballroom dancer.
Keeping fit for life
Her lifelong commitment to a healthy lifestyle began after she finished undergraduate studies at the University of Alabama at Birmingham.

Dr. Gerald with some of her powerlifting awards. She held state and national records, albeit briefly, in three categories. Among those was the strict bicep curl national record for her age group, which she won in 2013.
The apex of Dr. Gerald’s lifting career came when she placed second at the world championship in 2013. She was named the Arizona State 2013 Master Lifter of the Year after winning the state and national titles. She set state records in the squat (138 pounds) and bench press (110 pounds) and a national record for the strict bicep curl (77.15 pounds). The records didn’t stand long, she admits.
“It was for a very short period of time, and I'll just say there were not many of us in the older ladies category. So, yes, I do enjoy weightlifting a lot. But, since then, I've had a hip replacement (in 2018) and knee issues, so I'm not competing anymore,” she said.
These days, she still lifts and does CrossFit, but has narrowed her professional portfolio.
Asthma inhaler outreach
In her own research she has focused on improving asthma care in schools for 25 years. Dr. Gerald is a nationally-recognized expert and helped get a 2017 law passed in Arizona to allow any school employee to dispense stock inhalers to any child in respiratory distress. A stock inhaler is one that is not prescribed to a specific child and can be used by any child at the school.
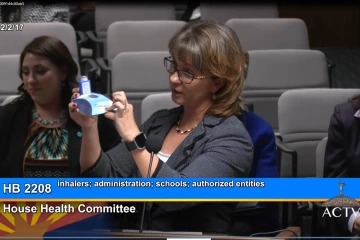
Dr. Gerald testifies at the Arizona State Legislature in 2017 to promote wider adoption of stock inhaler programs for students suffering from asthma in schools statewide and loosening rules on who could administer them.
Dr. Gerald consults on enacting or updating similar laws in other states. Seventeen states have adopted such measures, up from seven since Arizona passed its version. She most recently testified in Texas and Maryland, and counts Utah and Illinois among recent successes. For this, she was recognized in February as presenter of the 2022 Robert F. Lemanske, Jr, MD, FAAAAI Lectureship at the American Academy of Allergy, Asthma and Immunology (AAAI) annual conference, as well as with the UArizona Distinguished Outreach Faculty Award last year.
What interests her about asthma, she said, is that so many treatments work well but getting people to take those medications daily is a heavy lift. So, too, is getting them to avoid activities or situations that act as triggers. And many sufferers don’t always keep inhalers available with them.

During her sabbatical, Dr. Gerald will explore research methodologes to improve public adoption of best practices recommended in pulmonary studies.
“One of the fun things about stock inhalers for me is that I was the band booster president for my son's high school band at Catalina Foothills. He’s now a music ed major at ASU. But we had the largest band in the state with about 200 kids,” Dr. Gerald said. “And, so, of course, 10% of them were going to have asthma. And every time we had a practice or a performance, I was in charge of medications. There would be five kids having an asthma exacerbation and nobody had their inhaler,” so the stock inhaler legislation allowed her to provide one.
A Birmingham, Ala., native, she began researching asthma as a junior faculty member at UAB under Bill Bailey, MD, founder of the Lung Health Center, and one of the first researchers to receive NHLBI funding to study asthma in schools.
“I started helping on several of his studies and just fell in love with school-based asthma work. I realized how much there was to do, how different schools in my own town were for some kids than they were for me, and what a difference a school can make in kids’ health,” Dr. Gerald said.
Sabbatical goals
For her sabbatical, she plans on reading, taking online courses and traveling to learn the latest about “implementation research.” First, though, she’ll celebrate her 32nd wedding anniversary – also this July – with Joe Gerald, MD, PhD. A colleague at the Zuckerman College of Public Health, he was the chief compiler of the weekly Arizona COVID-19 forecast data used to guide decision-makers statewide. He is a frequent co-author with her on published papers.
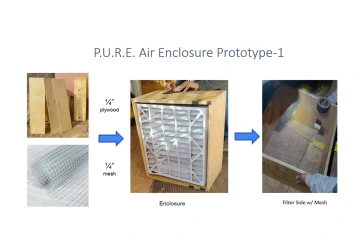
An ongoing box fan filter prototype project Dr. Gerald received funding for will help a larger effort to reduce pediatric asthma disparities on the Navajo Nation. Reservation child asthma rates run 14-18% versus 10% nationally, she said. Prototype partners include UC Berkely and Navajo Technical University.
Implementation research, Dr. Lynn Gerald said, involves study of methods to promote systematic uptake of proven clinical treatments, practices, organizational and management interventions into routine practice to improve health. That includes ways to encourage greater asthma inhaler use adherence.
“That’s really what I’ve done my entire life, trying to get interventions to work in a community setting outside of a clinical trial. But the methodology and things about how to do implementation science have changed a lot, so I’m going to be looking into that,” she said.
Dr. Gerald also will continue work with her own ongoing research projects, including one funded by a small grant from the Southwest Environmental Health Sciences Center at UArizona to develop a box fan filter prototype for use on the Navajo Nation to reduce air particulate from wood cook stoves in common use in rural areas. Partners include the University of California, Berkeley, and Navajo Technical University in Crownpoint, N.M., which will produce the filters.
“You just take the box fan, put a filter on it and you get a very inexpensive solution. It looks like this can reduce indoor air pollution from cook stoves by about 90%. This is a huge issue for Navajo kids and adults with respiratory problems. For many years, people have been trying to improve that situation, including stove exchange programs to put in newer, cleaner and more efficient ones,” Dr. Gerald said.
“What’s cool about this is it’s cheap. It’s developed and produced locally. And people can use their stoves the way they’ve always used them. Our long-term goal is to win a larger grant to see if we can further reduce the indoor air contamination to improve asthma outcomes for kids and adults there.”

