Can AI and a smartphone improve mental health treatment?
A graduate student is creating AI models to analyze smartphone data and detect behavioral changes that could lead to timely intervention and treatment.
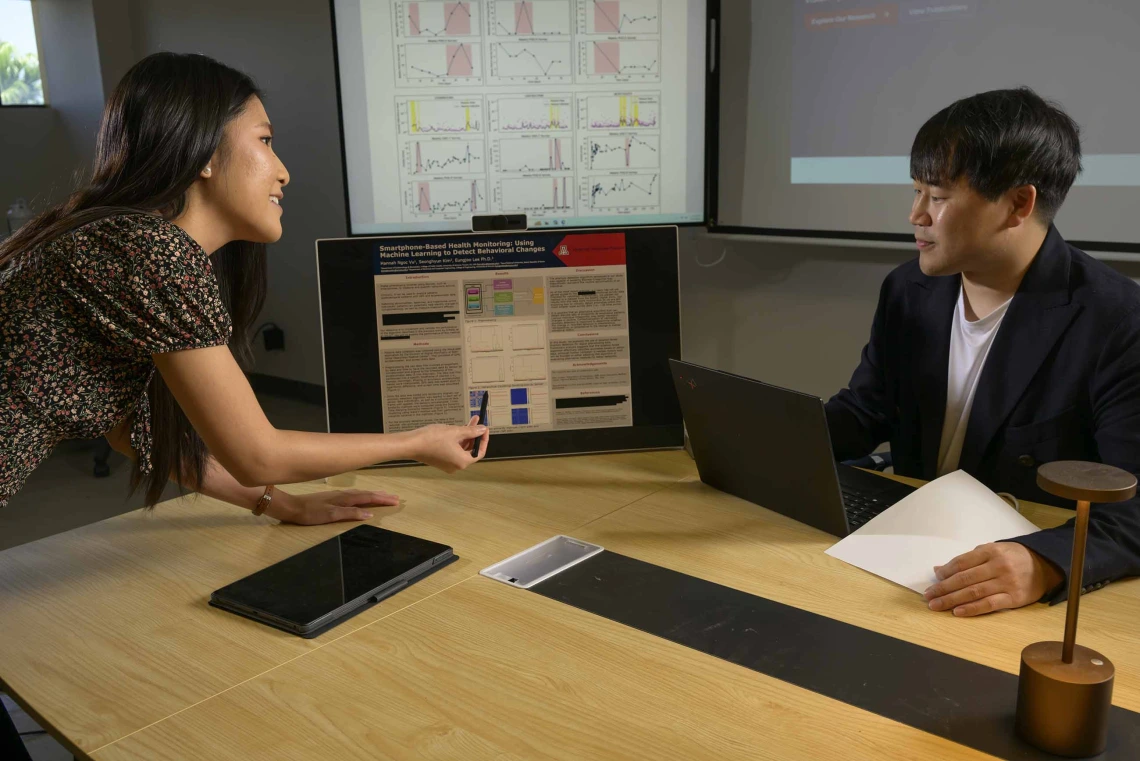
(From left) Hannah Vu, a graduate student in the Zuckerman College of Public Health, and her faculty mentor, Eung-Joo Lee, PhD, an assistant professor in the College of Engineering’s Department of Electrical and Computer Engineering, are combining their skill sets to apply artificial intelligence to health care.
Photo by Kris Hanning, U of A Health Sciences Office of Communications
Top takeaway:
- A University of Arizona Health Sciences graduate student is using AI and smartphone data to identify anomalies in behavior and track mental health, which could help patients and clinicians recognize worsening mental health for timely support.

Hannah Vu used machine learning to analyze smartphone data and detect behavioral anomalies that could be used for mental health interventions.
Photo by Kris Hanning, U of A Health Sciences Office of Communications
For people living with mental health conditions such as depression, obsessive-compulsive disorder or substance use disorder, the hardest part of managing their illness can be recognizing when things are getting worse and asking for help. But what if their phone could do that for them?
That is the idea behind a research project led by Hannah Vu, a graduate student in the University of Arizona Mel and Enid Zuckerman College of Public Health. Vu is working under the mentorship of Eungjoo Lee, PhD, an assistant professor in the Department of Electrical and Computer Engineering at the U of A College of Engineering, to develop an artificial intelligence-based tool to detect behavioral changes associated with mental health illness using data from smartphones.
The project is part of a broader push to harness AI in digital phenotyping – the practice of collecting active and passive data from personal devices – to detect subtle shifts in behavior that may signal worsening mental health.
“This is about empowering people who may not be able to advocate for themselves,” Vu said. “We’re looking at spatial-temporal data, like where someone is, how much they’re moving, how often they’re using their phone. That information can be valuable in tracking behavior over time. By measuring patterns in things like smartphone use and GPS location, we can give people a tangible way to see how they’re doing and track whether their treatment is helping.”
Finding patterns in data
Vu, who is pursuing a master’s degree in public health with a concentration in epidemiology, brings a unique perspective to this work. Her undergraduate background in physiology gave her a foundation in the biology of health, but she found herself increasingly drawn to behavioral health and the tools needed to study it.
Lee enjoys believes the combination of AI, engineering and health sciences can lead to more real-time disease detection tools for enhanced patient care.
Photo by Kris Hanning, U of A Health Sciences Office of Communications
“I wanted to study behavior, and I think it’s really important to approach it in a more computational way,” she said. “As an undergrad, I didn’t have the chops or the skill set to do those things, which is why I thought epidemiology might be a good pivot point. I could still use my physiology background and learn to think more statistically.”
That mindset drives her current work, looking for shifts in daily behavior that might otherwise go unnoticed. Vu’s project focuses on processing and analyzing sensor data collected passively from smartphones, including screen usage, GPS location and accelerometer readings. The information is captured by the mindLAMP smartphone app, developed at Beth Israel Deaconess Medical Center, a Harvard University-affiliated hospital.
Vu’s system uses this data to identify moments of change when someone’s behavior deviates significantly from their normal pattern. For example, someone with depression might gradually spend more time at home, stop meeting with friends or reduce the time they spend actively moving. A person with OCD may begin engaging in repetitive behaviors, which could show up as constant web searches or frequent texting.
“These anomalies might reflect the onset of a depressive episode or some other shift in mental state,” Vu said. “We want to compare them to mood surveys and patient anecdotes to see what those deviations actually mean.”
From code to clinic
The heart of Vu’s computational analysis relies on two machine learning tools: dynamic time warping and isolation forest. Dynamic time warping finds similarities and differences in data over time; An isolation forest is a clustering algorithm used to detect outliers.
“In a large dataset, most data points form a clear pattern or cluster, and the isolation forest algorithm helps identify the ones that fall outside that cluster. Those are the ones that could be clinically relevant,” Lee said. “It’s a way of recognizing when a person’s behavior changes in a statistically meaningful way.”
The research team will be validating the model by using mood surveys and clinical notes to interpret whether the anomalies correspond to meaningful changes in mental health status.

Lee’s primary research focuses on developing deep learning algorithms that utilize computationally efficient models designed specifically for embedded computer vision systems and medical imaging applications.
Photo by Kris Hanning, U of A Health Sciences Office of Communications
“Does this actually reflect what the person was experiencing at that time? Did they have a bad day, or a breakthrough moment, or a panic attack?” Vu said. “Those details are key to understanding what the data is telling us.”
Vu’s project is already laying the groundwork for future studies. In June, Vu and Lee traveled to Boston to meet with their collaborators at Beth Israel Deaconess Medical Center and explore new research ideas. One includes using social media data as an additional source of information to expand their anomaly detection work.
“They shared a few new datasets with us,” Vu said. “One of the interesting ideas they had was using our anomaly detection as a conversation aid. So, when a patient comes in, a provider could say, ‘Something unusual showed up here. What was going on at that time?’ It creates a chance to dig deeper.”
The team also discussed how machine learning might help fill gaps in incomplete datasets, allowing physicians to follow long-term behavioral trends with fewer blind spots. An algorithm, Vu said, could predict what might have happened during a time when smartphone data is missing.
Lee sees AI-based tools like this one and others being built in his lab not as replacements for clinical care but as foundations for improving it, particularly for patients who might otherwise fall through the cracks.
“AI will not replace clinicians, but it can give them tools to detect changes earlier and support better decisions,” he said. “This kind of passive data collection can also be scaled, since almost everyone already carries a smartphone.”
Vu believes that is part of what makes the approach so promising from a public health standpoint.
“If we can measure how behavior changes over time and in different environments, we can advocate for changes that are more sustainable,” she said. “It’s not just about the numbers; it’s about understanding what these anomalies mean in the context of people’s real-life experiences, validating how they're doing, and ultimately empowering them in their mental health journey."
Experts
Eung-Joo Lee, PhD
Assistant Professor, Department of Electrical and Computer Engineering, College of Engineering
Contact
Blair Willis
U of A Health Sciences Office of Communications
520-419-2979, bmw23@arizona.edu

