Fellowship helps a physician find her passion for treating chronic pain patients
Dr. Annie Lee, a recent graduate of the Pain Fellowship program, enjoys connecting with her patients and helping them manage their pain without opioids.
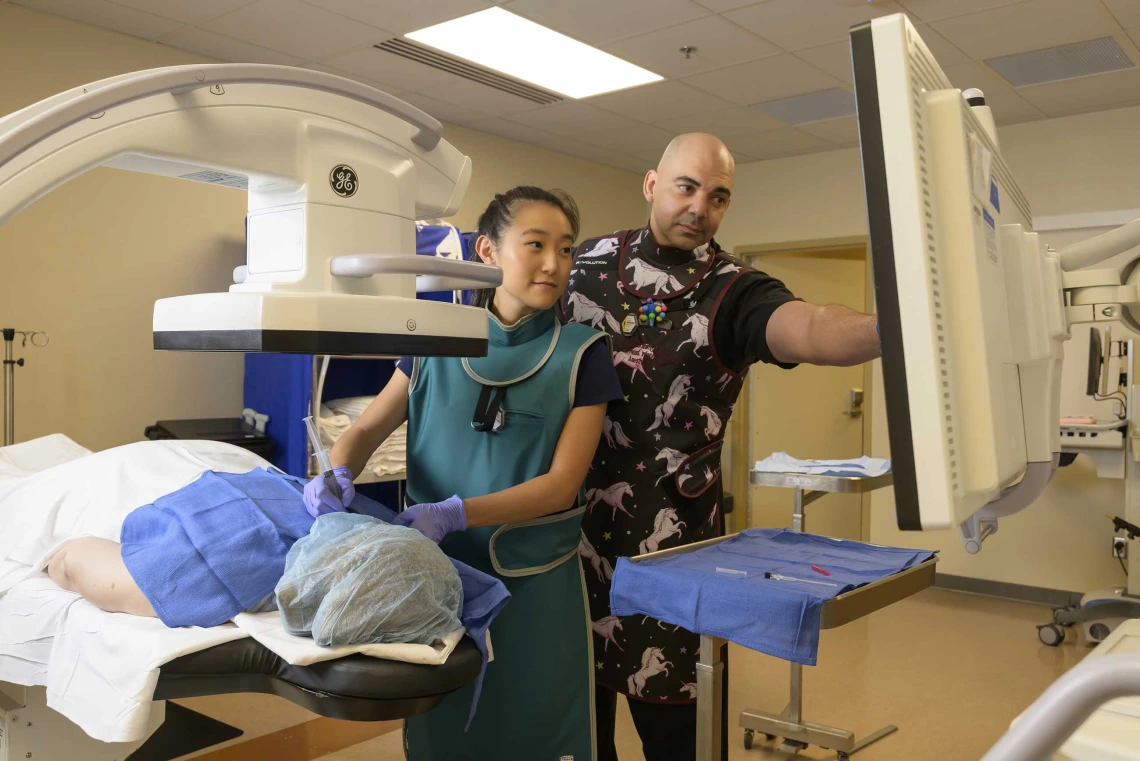
(From left) Annie Lee, MD, performed fluoroscopic-guided interventional pain management procedures under the watchful eye of Mohab Ibrahim, MD, PhD, as part of the Pain Fellowship program.
Annie Lee, MD, always knew she wanted to become a doctor.
“My first inspiration to go into medicine was definitely my two big brothers, who I always looked up to growing up,” said Lee, who was just 17 when she applied to Pennsylvania State University’s six-year accelerated program that led to her graduation from Jefferson Medical College (now the Sidney Kimmel Medical College) at the age of 24.

The first commencement Ann Lee, MD, celebrated with her parents, Jason and Mijung Lee, was her graduation from medical school. She didn’t attend her undergraduate commencement as she was already two years into medical school at the time.
Photo courtesy of Annie Lee, MD
Now 29, Lee found her professional niche in pain management thanks in part to a Pain Fellowship she completed under the direction of Mohab Ibrahim, MD, PhD, a professor of anesthesiology at the U of A College of Medicine – Tucson and director of the Pain Fellowship.
Ibrahim, who is also the medical director at the University of Arizona Health Sciences Comprehensive Center for Pain & Addiction, has been overseeing the Pain Fellowship since 2014, when the program only accepted one fellow per year. This year, Lee was one of the four fellows who graduated from the 12-month training program over the summer.
The fellows participate in patient care and become skilled in the evaluation and treatment of chronic and cancer pain while working in close collaboration with neurologists, neurosurgeons, orthopedic surgeons, physiatrists and psychiatrists. They become adept at using pharmacological and non-pharmacological interventional pain methods, including fluoroscopic-guided interventional pain management techniques such as somatic blocks, sympathetic blocks, neurolytic blocks, radiofrequency ablation, and spinal cord stimulator trials and implants.
At the conclusion of the fellowship, graduates are eligible to take the examination for the certification in pain management offered by the American Board of Anesthesiology.
“Millions of people in the U.S. are affected by chronic pain. The Pain Fellowship is one of the ways we can help patients by increasing the number of highly skilled doctors specifically trained to manage chronic pain,” Ibrahim said, adding that he is in the process of expanding the program to accept five fellows each year. “In the future, collaborations with the Comprehensive Center for Pain & Addiction will allow us to include the fellows in research and scholarly activities that will keep them on the cutting edge of treatments for chronic pain.”
Pain medicine: a growing field
Any physician can practice some pain management techniques, including prescribing medications for pain or performing procedures such as joint injections aimed at reducing a patient’s pain. But to be a pain physician, a doctor must complete a one-year pain fellowship accredited by the Accreditation Council for Graduate Medical Education.

As a young child, Lee (right) was inspired to become a doctor by her brothers, David (left) and John (center), who are both physicians.
Photo courtesy of Annie Lee, MD
In 2022, out of more than 989,000 physicians in the United States, only 6,778 specialized in pain medicine and pain management, according to the American Medical Association’s Physician Professional Data. National Residency Matching Program data for the last five years shows that pain medicine is among the top 20 most competitive subspecialty fellowships.
“A physician has to finish their residency training, and if they are interested in pursuing further education and training in the field of chronic pain management, they go into fellowship training to become pain physicians,” Ibrahim said, adding that he receives applications each year from physicians whose residencies were in a variety of fields, most commonly anesthesiology, but also neurology, psychiatry, emergency medicine, radiology, and physical medicine and rehabilitation.
Lee’s path to the Pain Fellowship was through anesthesiology. As a medical student, though, that wasn’t initially the specialty she thought she would pursue. Instead, she was leaning toward medicine or surgery.
“When I did my anesthesia rotation, I realized that it fit my personality best,” Lee said. “People have this idea that anesthesiologists get to put their patient to sleep, hang out for a couple hours and then wake them up. It’s so much more than that. Of course, we do put the patient to sleep, but a lot of anesthesia is being able to take care of that patient during that time. You really get to be there as a protector for the patient, which is what drew me to anesthesiology initially.”
After medical school, Lee took a residency position at the University of Southern California, where she spent four years learning the intricacies of anesthesiology and honing her skills in the operating room. She enjoyed the work tremendously, seeing it as a combination of her two favorite subjects from med school, physiology and pharmacology.
“I think that being a good chronic pain physician really involves being able to empathize and sympathize with your patients and to really care about them.”
— Annie Lee, MD
What she didn’t expect was the satisfaction she got from the brief moments before surgery, when she got to talk to her patients. Lee realized that in addition to making sure a patient was physically ready for surgery, she needed to meet their emotional needs.

Lee (right) was drawn to the U of A College of Medicine – Tucson’s Pain Fellowship program partially because of the opportunity to work with and learn from Mohab Ibrahim, MD, PhD, director of the Pain Fellowship program and the Banner – University Medical Center’s Pain Clinic.
Photo by Kris Hanning, U of A Health Sciences Office of Communications
“Patients place a lot of trust in you during surgery, because they’re completely asleep and vulnerable,” Lee said. “During those few minutes before surgery, when you get to talk to a patient, it’s a task to be able to connect with them during that time – really connect with them – and make them feel safe. As an anesthesiology resident, I really got to experience that responsibility and honor of taking care of somebody in their most vulnerable time. I really loved the emotional connection that I made with people during those moments.”
Lee shared that revelation with her brothers, who are both anesthesiologists and practicing pain physicians. They encouraged her to explore additional training in pain management to see if it would be a good fit for her.
She took their advice and was drawn to the University of Arizona Health Sciences, in part because it is close to her home in Southern California, but also because of Ibrahim.
“I had heard good things about him. Dr. Ibrahim has a reputation – he’s very well published, and he’s a great doctor,” Lee said. “I knew he was very smart, and he trained at the best places. As a learner, that’s who you want to teach you.
“As I got to know him, I realized the picture’s a lot bigger than that. It’s very impressive to see the relationships he developed with his patients. You can tell his patients trust him. There are some patients who are just so happy to see him – it’s the highlight of their day to see Dr. Ibrahim, and how many doctors are really the highlight of their patient’s day?” Lee added. “I think that being a good chronic pain physician really involves being able to genuinely empathize and sympathize with your patients. And as I continue to become the doctor that I want to be, I want to be taught by people like Dr. Ibrahim, who share those same principles and beliefs.”
Learning to manage pain without opioids
Lee started her fellowship on Aug. 1, 2023, seeing patients and performing procedures under the mentorship of attending physicians at the Banner – University Medical Center Pain Clinic.
Ibrahim said that from the beginning, patients loved Lee. For Lee, the feeling was mutual.
“I think a lot of these patients are impressive in themselves,” Lee said. “Chronic pain patients are often in a very, very vulnerable state. Oftentimes, they have been struggling with pain for a while. They haven’t been listened to by some doctors. They’ve been treated in ways that didn’t necessarily make their pain better. These people are living with pain every single day, they have good reasons to have their pain, and a lot of them just deal with it. Despite their pain, they’re still kind to the people around them, and they still manage to have a positive attitude. It sounds cheesy, but I think that’s inspirational. I like being able to talk to these patients and be there for them in a way that other physicians or other people weren’t necessarily able.”
Research showed the presence of pain management physicians in a clinic can improve patient outcomes while reducing the use of opioids.
A unique aspect of the Pain Fellowship is that while Lee was learning how to manage patients’ chronic pain, she was also learning how to do it without relying on prescriptions for opioids. The Pain Clinic is an opioid-free facility.
In November 2018, Ibrahim and a small research team conducted a retrospective review of the role of a pain clinic staffed by fellowship-trained pain physicians in reducing pain and opioid use in chronic pain patients. They examined medical records from nearly 300 patients who were on chronic opioids at the time of their first treatment at the Banner – University Medical Center Pain Clinic, where they were treated with nonopioid medications and interventional pain procedures as necessary.

A casual graduation ceremony was held in July for the 2024 Pain Fellowship physicians: (from left) Samrath Singh, MD, Ann Lee, MD, and Bardia Azar, MD.
Photo courtesy of Annie Lee, MD
Records were examined or 18 months, during which time pain scores reported by the patients decreased by 33.8%. The pain frequency and number of pain episodes improved, as did the ability to sleep, work and perform daily chores. Total opioid use decreased by about 55.4%.
“There are so many risks involved with opioids, and obviously, there’s an epidemic going on. I’m comfortable not prescribing a lot of opioids to my patients because I think that is oftentimes what is better for them,” said Lee, who did a few rotations at the University of Southern California’s opioid-free pain clinic during her residency. “I am grateful that I did my fellowship at an opioid-free clinic, because I think that we more specifically target the etiology of the patient’s pain and treat it from that perspective.”
And when it comes to treating chronic pain, Ibrahim said Lee is one of the best fellows the program has ever had.
“Annie has the capacity to connect with her patients. She is compassionate, and she always has a smile on her face,” Ibrahim said. “She’s very appropriate with her patients. She puts them at ease, whether it’s in the clinic or doing procedures. She’s kind-hearted, and I think her patients will be lucky to have her.”
With the Pain Fellowship behind her, Lee returned home to Southern California. After taking a short break to spend time with her family, she hopes to find a position that will allow her to pursue her love of anesthesiology and pain medicine.
“Chronic pain is not dramatic like anesthesiology can be, where the patient’s blood pressure can be dropping and the situation feels like life and death,” Lee added. “But I do think with chronic pain, you get to save people’s lives in a lot of ways, because you’re really changing their quality of life.”
Our Expert
Mohab Ibrahim, MD, PhD
Professor, Department of Anesthesiology, College of Medicine – Tucson
Program Director, Pain Medicine Fellowship, College of Medicine – Tucson
Director, Chronic Pain Management Clinic, Banner – University Medical Center
Medical Director, Comprehensive Center for Pain & Addiction, U of A Health Sciences
Contact
Stacy Pigott
U of A Health Sciences Office of Communications
520-539-4152, spigott@arizona.edu

