Removing barriers to high-quality opioid use disorder care
A nurse-scientist hopes to empower primary care nurse practitioners to play a crucial role in improving access to evidence-based care for patients with substance use disorders.

Nurse practitioners play a vital role in health care, but their ability to effectively treat patients with opioid use disorder can be limited by myriad factors, according to researchers at the University of Arizona Health Sciences.
Photo by Martin Barraud via Getty Images

Zhanette Coffee, PhD, MSN, APRN, is member of the U of A Health Sciences Comprehensive Center for Pain & Addiction and a postdoctoral research associate at the College of Nursing.
Photo by Kris Hanning, U of A Health Sciences Office of Communications
Zhanette Coffee, PhD, MSN, APRN, spent years working as an advanced practice nurse with certifications in family practice and addictions nursing and saw firsthand the challenges faced not only by patients with opioid use disorder, but also by the health care professionals providing treatment to those patients.
“I grew up with a parent who struggled with substance use, chronic pain and mental health,” said Coffee, who is now a member of the Comprehensive Center for Pain & Addiction at the University of Arizona Health Sciences. “When I started working specifically in the substance use field, I quickly realized my deep passion for it. Having grown up witnessing these struggles firsthand and later caring for individuals facing similar challenges, my commitment to this work was solidified. We need better solutions. We need innovative, compassionate approaches to effectively treat this vulnerable population.”
In 2021, research showed that only 22% of approximately 7 million Americans with opioid use disorder received evidence-based treatment. That gap in care is widened by a critical lack of providers in primary care, mental health and addiction medicine.
As a nurse practitioner, Coffee was already filling a critical need for skilled health care providers to treat substance use disorders, but her experiences ignited a passion within to do more. She wanted to break down barriers and improve patient care.
Watch Zhanette Coffee, PhD, MSN, APRN, talk about her path from nurse to nurse-scientist.
“My nursing career really gave me that firsthand clinical insight and immersed me in the field,” Coffee added, “but I realized I wanted to be on the other end of developing interventions to really shift addiction science and improve outcomes for patients.”
Breaking down the barriers
With that goal in mind, Coffee found herself at the U of A College of Nursing, where she earned her doctorate and is now a postdoctoral research associate. She hit the ground running as a new researcher. Her first paper, “Empowering Primary Care Nurse Practitioners: A Multilevel Approach to Combating the Opioid Crisis,” was published in late December in the Journal of Advanced Nursing.
The position paper was designed to drive change at the individual level (nurse practitioner), the dyadic level (provider-patient relationship), and the systems level (organizational culture, education and policy). The end goal is to strengthen nurse practitioners’ capacity to deliver optimal care for opioid use disorder.
“Access to evidence-based treatment remains a significant barrier for people in the United States with opioid use disorder,” said Todd Vanderah, PhD, director of the Comprehensive Center for Pain & Addiction and Regents Professor and head of the Department of Pharmacology at the College of Medicine – Tucson. “Dr. Coffee’s work in identifying barriers to care is a powerful first step in empowering nurse practitioners to deeply impact patient lives by transforming care for opioid use disorder.”
At the individual level, barriers to optimal opioid use disorder care included low motivation and personal acceptability to treat opioid use disorder. Nurse practitioners might be influenced by their experiences with a family member who was affected by alcohol or other drugs, beliefs about personal responsibility, perceptions of stigma, perceived danger, work experience or availability of continuing education on substance use, and other factors.
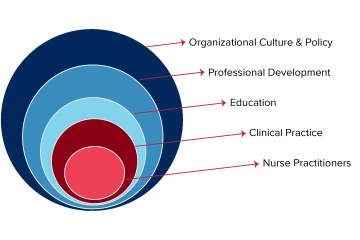
Coffee adapted the Advanced Practice Provider conceptual model to focus on a multilevel systems approach to augment nurse practitioners’ role and improve care for patients with opioid use disorder, beginning with strategies to enhance engagement and motivation for nurse practitioners and improve nurse-patient interaction, supported by organizational, education and policy refinement.
Illustration by Xinyu Zhang, U of A Health Sciences Office of Communications
The consequences can be severe, including higher recurrence of drug use among patients with opioid use disorder and an increased likelihood of patients discontinuing treatment prematurely.
“At the personal level, there can be low motivation, reluctance to treat this population or even ambivalence toward people who struggle with drug use,” Coffee said, explaining that addiction stigma results from the persistent and pervasive belief that addiction is a personal choice reflecting a lack of willpower or moral failing.
Stigma also rose to the surface as a significant dyadic barrier, not only within the provider-patient relationship but also between providers. Negative attitudes and views toward patients with opioid use disorder can extend to the providers who choose to care for them.
“Nurse practitioners often work in settings where colleagues may treat them differently or hold stigmatizing beliefs about providers specializing in addiction, questioning their credibility as clinicians,” said Coffee, who is a member of the university’s BIO5 Institute.
Negative provider-to-provider interactions can add job-related stress and be a symptom of poor organizational culture, both of which can lead to clinician burnout. Two cited research studies found that approximately 25.3% of primary care nurse practitioners report feeling burned out and nearly 46.2% of nurse practitioners report working in poor organizational climates.
“The area in which you work can really impact the quality and accessibility of how you can treat opioid use disorder, because administrators and leadership within that clinical setting can significantly impact your overall work environment and workplace support,” Coffee said.
Additionally, many nurse practitioners do not feel adequately trained to provide whole-person, evidence-based care for opioid use disorder. The standard generalized education training nurses receive varies significantly in how it addresses substance use disorders, Coffee said.
“What if the patient has chronic pain and they’ve been using opioids to manage their pain for a very long time? What if the patient is also struggling with mental health?” Coffee said. “Those are complex factors that you need training and support for in order to effectively treat that patient.”
Taking a stance to ignite change
Coffee wrote the paper with her mentors, Vanderah and Judith Gordon, PhD, professor emerita at the College of Nursing, as well as a broad national network of nurse-scientists with first-hand clinical experience treating opioid use disorder. The result was a position paper empirically informed by the authors’ personal experiences and supported and backed by the scholarly work of researchers around the world.

Coffee worked as a nurse in various hospital and clinic settings, including working with patients experiencing chronic pain and substance use disorders.
“There are multilevel factors that can hinder nurse practitioners from treating opioid use disorder. We have lived experience, and we recommend that academic and clinical settings develop a cross-sector response to the opioid crisis,” Coffee said. “We need to educate and train providers – especially new providers who are going into the workforce – and equip them to effectively treat substance use disorders.”
There were approximately 385,000 licensed nurse practitioners in the U.S. in 2023, according to the American Association of Nurse Practitioners. Coffee is one of only 1,484 nurses in the U.S. and Canada have completed the process to become a Certified Addictions Registered Nurse or Certified Addictions Registered Nurse-Advanced Practice, according to the Addictions Nursing Certification Board’s website.
“About 70% of nurse practitioners work in primary care. We’re a large workforce, and we are the No. 1 trusted profession,” Coffee said. “If a patient who is struggling with substance use disorder goes into primary care, they should be able to trust their provider to offer that care. This research sheds light on the barriers that prevent that from happening, especially for nurse practitioners.”
At the end of the day, Coffee is excited to think about the ways her paper could be used to invoke change. She believes nurse practitioners may find valuable insights to inform their own careers, while the overarching message posits a necessary shift in addiction medicine and science.
She launched her next study and is currently recruiting participants for a brief 10-minute survey exploring the barriers, facilitators and attitudes of nurse practitioners and advanced practice registered nurses in treating adults with opioid use disorder. She recently received a BIO5 Postdoctoral Fellowship to help fund the project.
“If providers face barriers, the patients will receive lower-quality and less effective opioid use disorder care,” Coffee said. “My experience treating patients, witnessing their recovery, and being deeply immersed in the field, both as a clinician and a researcher, continues to inspire me. We still have work to do, and as the science evolves, we must continue advancing solutions to better support this population and address the opioid crisis.”
Experts
Zhanette Coffee, PhD, MSN, APRN
Postdoctoral Research Associate, U of A College of Nursing
Member, Comprehensive Center for Pain & Addiction
Member, BIO5 Institute
Todd Vanderah, PhD
Regents Professor, Department of Pharmacology, U of A College of Medicine – Tucson
Director, Comprehensive Center for Pain & Addiction, U of A Health Sciences
Co-Director, MD/PhD Program, U of A College of Medicine – Tucson
Professor, Department of Anesthesiology, U of A College of Medicine – Tucson
Professor, Department of Neurology, U of A College of Medicine – Tucson
Member, BIO5 Institute
Member, U of A Cancer Center, U of A Health Sciences
Contact
Stacy Pigott
U of A Health Sciences Office of Communications
520-539-4152, spigott@arizona.edu

