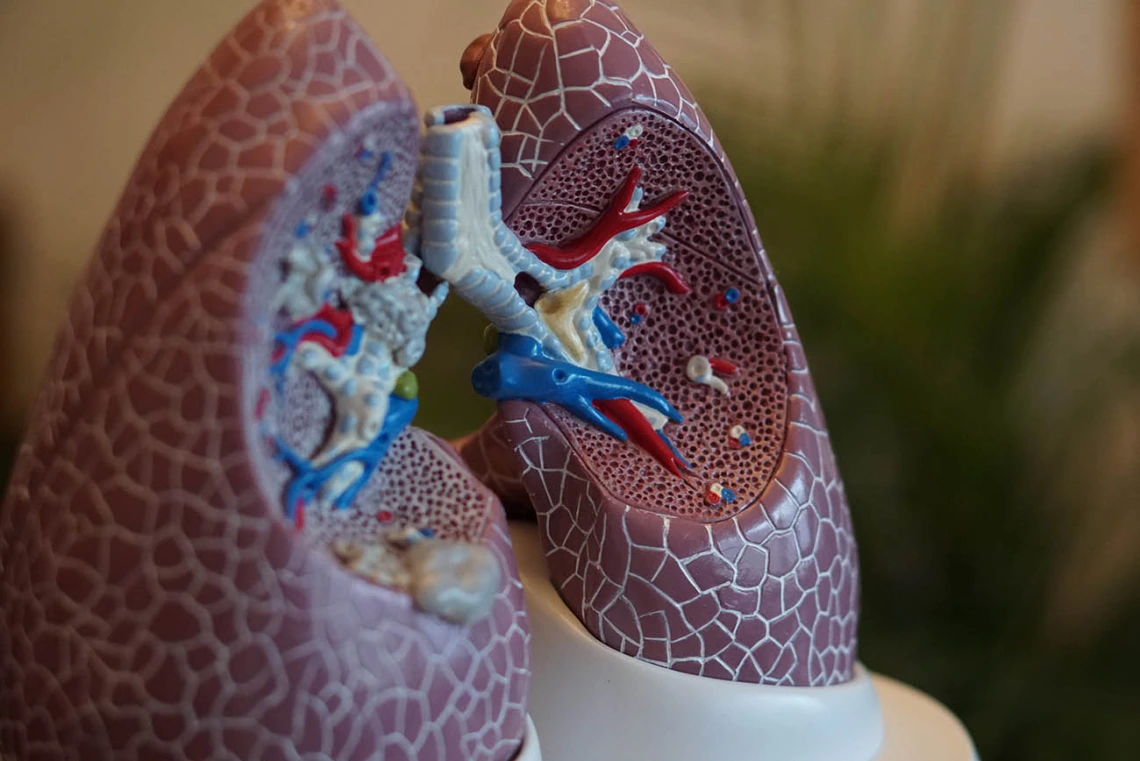
Characterizing Emphysema Immune Responses May Lead To Personalized Treatments for COPD
With a $3.3 million grant from the National Institutes of Health, Dr. Francesca Polverino will investigate B cell responses in patients with emphysema.
Research led by Dr. Francesca Polverino and collaborators will explore the link between unique immune responses and chronic obstructive pulmonary disease (COPD).
A $3.3 million National Institutes of Health grant will allow University of Arizona Health Sciences researchers to characterize the unique immune response associated with emphysema, a lung condition that causes shortness of breath and often leads to chronic obstructive pulmonary disease (COPD), ultimately informing earlier and more personalized treatment approaches.

Francesca Polverino, PhD, is leading a research team that will examine the immune responses of patients with emphysema in an effort to develop personalized treatments for COPD. (Photo: University of Arizona Health Sciences)
“People with emphysema cannot be encompassed under the same umbrella as other COPD patients because they present a completely different disease,” said Dr. Polverino, also an associate research scientist with the UArizona Asthma & Airway Disease Research Center.
Unlike those with chronic bronchitis, emphysema patients exhibit autoimmune responses leading not only to loss of lung tissue, but also to loss of bone and muscle throughout their bodies. These patients are “falling apart systemically,” Dr. Polverino says, likely because of improper B cell responses.
B lymphocytes, a key part of the adaptive immune system, are white blood cells responsible for producing antibodies in response to foreign materials and harmful microbes. While the actions of B cells are essential to our protection against a variety of diseases, they sometimes incorrectly target our own tissues, leading to an autoimmune response.
Prior research by Dr. Polverino and others has shown that not all COPD patients – only those with emphysema – have prominent lung B cell responses, regardless of the degree of airflow limitation they experience.
With this five-year grant from the NIH’s National Heart, Lung, and Blood Institute, Dr. Polverino and her team will further explore the B cell immune responses in COPD patients, especially those with emphysema and heightened autoimmunity. They aim to identify biomarkers of emphysema B cell responses that are distinct from other types of COPD, allowing scientists and physicians to take a precision medicine approach to treating this chronic disease.
“This research is the first brick of a wall because we really don’t know anything about the B cell response in these people,” Dr. Polverino said. “This work is very overdue.”
Once she correlates the extent of B cell activity with emphysema severity, Dr. Polverino plans to assess antibody production throughout the body, as emphysema can cause systemic (whole-body) problems. If her hypothesis is correct, Dr. Polverino expects that circulating off-targeted B cells, similar to that in the lung, will also correlate with emphysema severity.
COPD is a progressive, inflammatory disease that is multifactorial in nature with not only environmental contributors, but genetic and developmental factors, as well. Tobacco smoke is the most prominent risk factor in developed countries like the U.S., while inhalation of smoke generated by burning fuels indoors is key for underdeveloped countries around the globe.
Current treatments including lifestyle changes, prescription medication, breathing therapies and surgery are used for both. So far, a therapy modifying the course of COPD has not been found.
Dr. Polverino, an expert in chronic lung diseases, will lead the research team that includes scientists from UArizona and other institutions. Her UArizona collaborators include: BIO5 member Deepta Bhattacharya, PhD, also an associate professor of immunobiology, who will conduct functional B cell assays; Paul Langlais, PhD, an associate professor of medicine and director of the UArizona Proteomics Lab, who will assist with the use of a mass spectrometer, a tool used to determine the precise components of a substance; Darren Cusanovich, PhD, another BIO5 member and assistant professor of cellular and molecular medicine, who will perform single-cell sequencing to determine the genetic differences between B cells in COPD patients; and Jin Zhou, PhD, associate professor of epidemiology in the UArizona Mel and Enid Zuckerman College of Public Health, who will assist Dr. Polverino with biostatistical analyses.
This study is funded by the National Heart, Lung and Blood Institute, a division of the National Institutes of Health (R01HL149744.)
Contact
Brittany Uhlorn, PhD
214-783-7397
bforte2012@bio5.org

