MD/PhD Student Offers New Approach to Make Walking Easier for Children with Cerebral Palsy
Third-year student’s Scholarly Project research taps into his biomechanics background to improve and test robotic exoskeleton therapy.

Third-year MD/PhD student Ben Conner is studying a robotic walking therapy for children with cerebral palsy.
A University of Arizona College of Medicine – Phoenix student is helping children with cerebral palsy improve their mobility by having them train using a robotic exoskeleton.
Third-year MD/PhD student Ben Conner is studying a robotic walking therapy for children with cerebral palsy for his scholarly project requirement. His research is part of an interdisciplinary team housed at Northern Arizona University’s Biomechatronics Lab, which is led by Zachary Lerner, PhD, assistant professor, Department of Mechanical Engineering. The lab seeks to restore neuromuscular function and augment human ability through the design, control and testing of robotic exoskeletons.
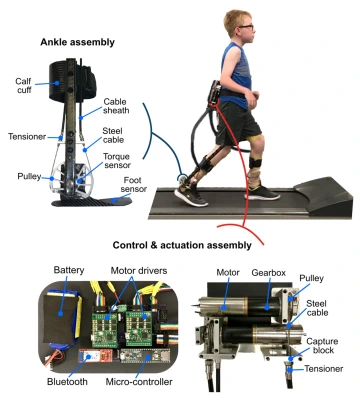
Using motors and a wireless control system worn at the waist, the exoskeleton works with muscles in the legs to propel the body forward.
With custom designs and control schemes, the lab’s exoskeletons can serve multiple purposes. An assistive feature is designed to make walking easier for kids with cerebral palsy (CP). Using motors and a wireless control system worn at the waist, the exoskeleton works in concert with muscles in the legs to propel the body forward and create a more normal walking pattern. Conner’s project, on the other hand, is focused on a resistive feature to serve as a therapeutic intervention.
“It’s a cool feeling how the exoskeleton takes over,” Conner said. “but we also wanted to offer a training feature so that ultimately these kids wouldn’t have to wear anything. That’s where we came up with our resistive feature and this training study.”
The resistive feature focuses on re-training signals between the brain and the muscles in the legs to work more efficiently while walking.
“Kids with CP are weaker than their typically-developing peers. This is due to both smaller muscles and an inability to effectively fire those muscles,” he said. “Using our device, we resist the push-off phase of walking so that the kids are forced to recruit greater muscular force in order to take a step. With repetitive practice, we have found that this carries over to greater strength and muscle recruitment while walking without the exoskeleton on, making these kids faster with greater endurance.”
Cerebral palsy inhibits controlled movement and often results in exaggerated reflexes, floppy or rigid limbs and involuntary motions. According to the CDC, it is the most common motor disability in childhood. About 1 in 323 children has been identified with CP.
The neurological disorder begins during infancy, resulting in limitations in activity that occur during a critical period of development when kids are supposed to be physically active, interacting with their peers and learning effective movement patterns for lifelong mobility. Without proper treatment, these limitations in activity can cause children with CP to lose the ability to walk by adulthood.
“Individuals with CP have a progressive decline of mobility, and that’s the issue we are trying to address. If you look at the research, walking ability is directly correlated to physical activity levels for this population. By enabling improved walking patterns with our exoskeleton therapy, we hope to make these kids more physically active, allowing them to get bigger and stronger, and keep up with their friends in school or on the playground.”
Conner is conducting his study at the Phoenix Biomedical Campus Rehab Lab in collaboration with the NAU Physical Therapy Department. His clinical advisor is Michael Kruer, MD, associate professor of Neurology and Child Health at the College of Medicine – Phoenix. A molecular geneticist, Dr. Kruer’s research focuses on the genetic basis of neurodevelopmental and neurodegenerative disorders in children.
Conner, under the supervision of Drs. Lerner and Kruer, has recruited children with CP from the local community to participate in his study. He starts participants with a baseline analysis of their strength, motor control and functional mobility. Conner then leads them through training sessions with the exoskeleton therapy, followed by a post-assessment to measure changes.
“It’s been a great learning experience. I’m able to tie in my clinical training from medical school as I interact with our participants and interpret results. Good bedside manner is essential to make this pediatric population comfortable with participating in our study, and the translation of our work relies on an understanding of underlying pathophysiology and the current standard of care,” Connor said.
“At the same time, I’ve been able to learn from the engineers in my lab to acquire important technical skills related to device design and control. Ultimately, I hope to bridge the gap between advances in technology and clinical care.”
Conner said his interactions with kids have left him struck by the unique challenges that can come with the movement disorder.
“Almost all of us, as kids, are given this opportunity to be active and healthy…from day one, most kids with CP are not given this same opportunity. To me, motion is medicine, and I want to find ways to make that possible for all kids, regardless of their diagnosis.” — Ben Conner, third-year MD/PhD student
Current treatments for those with CP usually include medications such as muscle or nerve injections and oral muscle relaxants, physical therapy and orthopedic surgery. The training device would work to supplement these treatments. The research lab hopes to ultimately make the device commercially available.
“Our ability to use a relatively inexpensive and mobile device to improve the connection between the brain and muscles for improved walking in kids with CP is new, and really exciting,” Conner said. “Building off what we’ve found in these initial studies, we aim to commercialize our device and make it accessible to these kids and their families.”

