Supercharging the Immune System: The Future of Cancer Care
Most people familiar with cancer treatment know of three main options: surgery, radiation and chemotherapy. But a newer option, called immunotherapy, is creating quite a buzz across the cancer community.

CAR T cell therapy provides a safety net for patients whose cancers return even after standard treatments.
Immunotherapy comes in many “flavors.” Some you may have heard of, like vaccines and bone marrow transplants. But other types are even more cutting-edge.
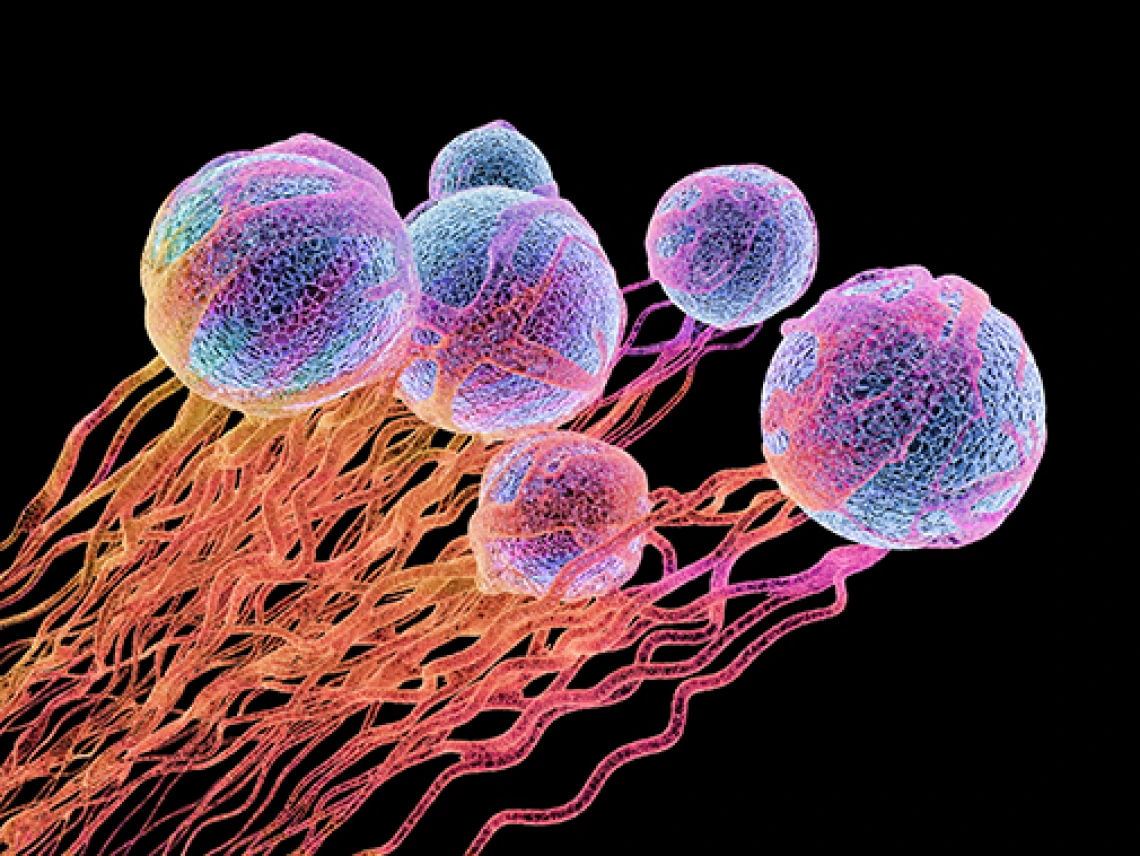
“Now we’re in the era of cellular immunotherapy,” says Daniel Persky, MD, director of the University of Arizona Cancer Center Clinical Trials Office. “We’re using cells, particularly T cells, which are being retrained or redesigned to fight cancers more directly.”
CAR T cells are a form of cellular immunotherapy that gained media attention and public excitement as the first cancer treatments to alter a patient’s genes. In 2017, the FDA approved two CAR T-cell therapies in quick succession: one for patients with advanced leukemia in August, and a second for patients with large B-cell lymphomas in October.
T cells are separated from the blood and “supercharged” with a gene that generates chimeric antigen receptors (CAR), which allow the T cells to bind to cancer cells and destroy them.
In general, immunotherapy drugs are not frequently used in pediatric populations. CAR T cells are an exception.
“CAR T cells are used to treat acute lymphoblastic leukemia, which is very common in kids,” says Emmanuel Katsanis, MD, director of the UA Cancer Center Blood and Marrow Transplantation Program.
This therapy provides a safety net for patients whose cancers return even after standard treatments.
“Bone marrow transplant still offers a cure for 75 to 80 percent of patients with acute lymphoblastic leukemia,” says Dr. Katsanis. “CAR T cells currently are reserved for patients who relapse, usually after bone marrow transplant.”

Most people familiar with cancer treatment know of three main options: surgery, radiation and chemotherapy. But a newer option, called immunotherapy, is creating quite a buzz across the cancer community.
“We’re bringing clinical trials with CAR T-cell therapy here,” reports Dr. Persky. “We will also be opening our cancer center to standard-of-care CAR T cells.”
In the future, additional research will reveal whether CAR T cells can be aimed at solid tumors like breast and colorectal cancers. The addition of further CAR T-cell therapies to the list of approved treatments also will help patients whose cancers have relapsed. With more research, trials and FDA approvals, the future of cancer treatment is only getting brighter.
Learn more about the promise of immunotherapy in the recent issue of Act Against Cancer, in which UA Cancer Center physicians and scientists discuss their work in this exciting new field.
About the Author
The University of Arizona Cancer Center is one of 45 comprehensive cancer centers in the nation and the only one headquartered in and serving the entire state of Arizona that has been designated by the National Cancer Institute as a Comprehensive Cancer Center, the NCI’s highest designation. That designation is reserved for centers focusing on patient care as well as basic and clinical research, prevention, education, outreach and training.
The Cancer Center is a leader in research on women’s cancers (breast, ovarian), men’s cancers (prostate), gastrointestinal cancers (colon, pancreas and liver), lymphoma and skin cancers and is home to one of the largest Cancer Prevention and Control Programs among the nation’s comprehensive cancer centers, with leading prevention research in breast, colon, lung, prostate and skin cancers.

