Identifying a Link Between Prolactin and Female Pain
Dr. Frank Porreca is looking for options to manage chronic pain in women by uncovering the selective actions of prolactin in female-prevalent pain disorders.
“People have studied sex hormones – primarily estrogen and testosterone – and pain for decades, but nobody's really understood how it works,” said Frank Porreca, PhD, whose research has identified prolactin as a potential therapeutic target for female-prevalent pain.
One of the biggest risk factors for pain is being female.
Migraine, fibromyalgia, rheumatoid arthritis, irritable bowel syndrome and many other pain disorders are more prevalent among women than men, though doctors and scientists have never understood why. University of Arizona Health Sciences researchers believe part of the answer might be found in prolactin, a hormone that is best known for stimulating milk production in women.
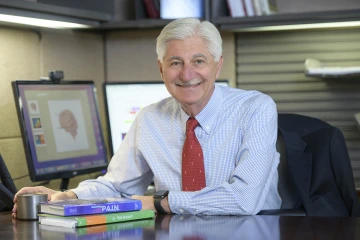
Frank Porreca, PhD, associate head of the College of Medicine – Tucson’s Department of Pharmacology and a member of the UArizona Health Sciences Comprehensive Center for Pain and Addiction, is examining the role prolactin plays in female-prevalent pain disorders, including migraine.
“Almost all pain disorders are female prevalent. If we are going to treat the majority of pain patients, we have to treat women. But how do you do that unless you know if there are mechanisms that can increase pain in females?” said Frank Porreca, PhD, who is a member of the UArizona Health Sciences Comprehensive Center for Pain and Addiction and the associate head of the College of Medicine – Tucson’s Department of Pharmacology. “Our research shows that prolactin, which is naturally higher in women than in men, changes the thresholds for activation of the nociceptors, which are the body’s pain receptors, only in females. It shows that female and male pain receptors are different, which is an incredible biological insight.”
The research, conducted by Dr. Porreca and Edita Navratilova, PhD, assistant professor of pharmacology, offers a first glimpse of the mechanisms by which prolactin contributes to migraine pain. Together, Drs. Porreca and Navratilova hope to develop preventive and therapeutic options specifically for women to manage chronic pain.
Migraine: a starting point
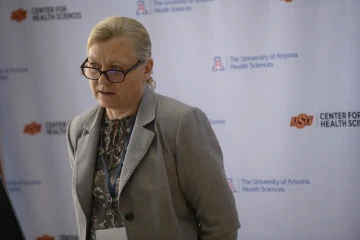
Edita Navritalova, PhD, assistant professor in the Department of Pharmacology in the College of Medicine – Tucson, collaborates with Dr. Porreca on research into prolactin and other mechanisms of acute and chronic pain.
Decades of research into migraine have identified a few characteristics of the complex neurological condition.
- Migraine is female prevalent.
- Migraine is multiphasic.
- Migraine headaches are associated with triggering events.
Migraine, which is three times more likely to affect women than men, progresses through different stages: premonitory, also known as prodrome; aura, which approximately one-third of people experience during a migraine attack; headache or main attack; and recovery or postdrome.
“Nobody can agree on what triggering events are, but patients often self-report that stress is a triggering event,” Dr. Porreca said, adding that stress can take many forms, including work deadlines, lack of sleep, menstrual cycle changes, or poor nutrition or hydration.

About three out of four people who have migraines are women, according to the Office on Women's Health at the U.S. Department of Health and Human Services.
Stress activates the hypothalamus, located deep within the brain. The hypothalamus is the main link between the endocrine system, composed of glands and the hormones they secrete, and the nervous system, which includes neurons, or nerve cells, that transmit signals to different parts of the body. Afferent neurons, also called sensory afferents, transmit information such as smell, taste, temperature and pain signals from the outside world into the brain.
Doctors and scientists know the hypothalamus is also activated during the premonitory phase of migraine, but it is unclear how that activation transitions into pain.
From prolactin to pain
“One of the hypotheses in migraine is that the reason the pain attacks happen is the threshold for activation of sensory afferents goes down,” Dr. Porreca said. “If you have a lower threshold to activate, then things that shouldn't produce the pain, now do.”
“Our continuing research helps us understand why the majority of pain patients in the world are female”
Frank Porreca, PhD
Dynorphin, an endogenous opioid peptide that is involved in learning, memory and emotional control, is a key part of the body’s stress response. Dynorphin activates the kappa opioid receptor circuit in the hypothalamus, starting a series of events that results in even more prolactin being released.
To test the effects of high levels of prolactin on sensory afferents, Dr. Porreca and his research team blocked the release of prolactin in response to stress or kappa opioid receptor activation in animal models.
“When prolactin is elevated, it lowers the response thresholds of the sensory afferents, and, interestingly enough, it does so in female but not in male animals,” Dr. Porreca said of the findings that were published in the journal Brain in March.
“This gives us insight into how brain stress circuits connect with the sensory afferents through a neuroendocrine mechanisms that promotes pain selectively in females,” he added. “Now we know in females there is a mechanism that doesn't exist in males, and that mechanism may increase the likelihood that something innocuous can trigger a migraine.”
Potential paths to a therapeutic

(From left) Drs. Frank Porreca, Yanxia Chen (who was a doctoral student at the time), Edita Navratilova, Aubin Moutal and Rajesh Khanna all worked on the paper that was recently published in BRAIN. The team previously published research that was featured on the cover of Science Translational Medicine.
Dr. Porreca’s research into prolactin is continuing thanks to a $2.3 million grant from the National Institute of Neurological Disorders and Stroke, a division of the National Institutes of Health. The project, “A prolactin-mediated neuroendocrine link between stress-induced latent sensitization and female-selective pain,” seeks to further unravel mechanisms for therapeutic interventions, allowing for improved therapy of functional pain syndromes in women. The research team includes Dr. Navratilova and Volker Neugebauer, MD, PhD, of the Texas Tech Univeristy Health Sciences Center School of Medicine.
Dr. Porreca is particularly excited about the potential of prolactin antibodies to treat migraine. Prolactin antibodies are already being researched for a variety of applications including endometriosis and breast cancer. Dr. Porreca is collaborating with Peptide Logic LLC, a biopharmaceutical company founded by Pierre Rivière, PhD, one of his former postdoctoral researchers, to develop a prolactin antibody for pain.
“Our continuing research helps us understand why the majority of pain patients in the world are female and possibly helps explain the female prevalence of migraine,” Dr. Porreca said. “While our research was about migraine, truthfully, this could apply to any female-prevalent pain disorder.”
Our Experts
Contact
Stacy Pigott
520-539-4152
spigott@arizona.edu

