Reducing Atrial Fibrillation’s Fear Factor
It’s a common scenario in a cardiology clinic when the cardiologist informs the patient they have atrial fibrillation (AFib), an abnormal heart rhythm characterized by rapid and irregular beating.

It’s a common scenario in a cardiology clinic when the cardiologist informs the patient they have atrial fibrillation (AFib), an abnormal heart rhythm characterized by rapid and irregular beating. Shock and fear take over, especially once the cardiologist says something about “increased risk of stroke.”
Most likely the patient or the adult children will go online to learn more. (We know this because the University of Arizona Sarver Heart Center “Heart Rhythm” health page is one of the most visited sections of our website.) And, that’s smart since no one wants to have a stroke.
Atrial fibrillation, the most common heart rhythm abnormality, affects about 3 million individuals in the United States, with the number projected to increase as our population ages. Half of these patients will be 80 years or older.
These patients often have other conditions, such as high blood pressure, heart failure or heart-valve disease. Recently, obesity and obstructive sleep apnea have been recognized as new risk factors. Research has disclosed genetic defects that predispose families to atrial fibrillation.
The stroke risk for AFib patients is real – about one-fifth of the approximate 500,000 strokes in the United States (per year) are related to atrial fibrillation – but these are largely preventable. The risk of AFib-related stroke depends on a variety of factors, including age and other specific medical problems, like hypertension and diabetes. The decision to recommend anticoagulation (blood thinners) is tailored to the individual after a detailed discussion with your physician. There are several options for anticoagulants, including several newer alternatives to Coumadin®, also known as warfarin.
In addition to the risk of stroke, many people with AFib suffer from symptoms like breathlessness, a lack of endurance and irregular or rapid heart palpitations. A minority of patients also may develop heart failure related to AFib that can resolve with control of the rhythm. People who have been in AFib for a longer duration may have subtler symptoms, often attributing their lack of stamina, from: age or other environmental factors. Restoring normal rhythm in many of these people can have a significant impact on their level of function.
Here are other ways atrial fibrillation is treated:
Electrical cardioversion, or delivering electrical shock to the chest under anesthesia, can revert atrial fibrillation to normal rhythm; however, to maintain normal rhythm many people will need to take daily rhythm control medications.
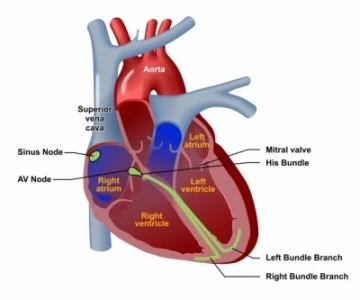
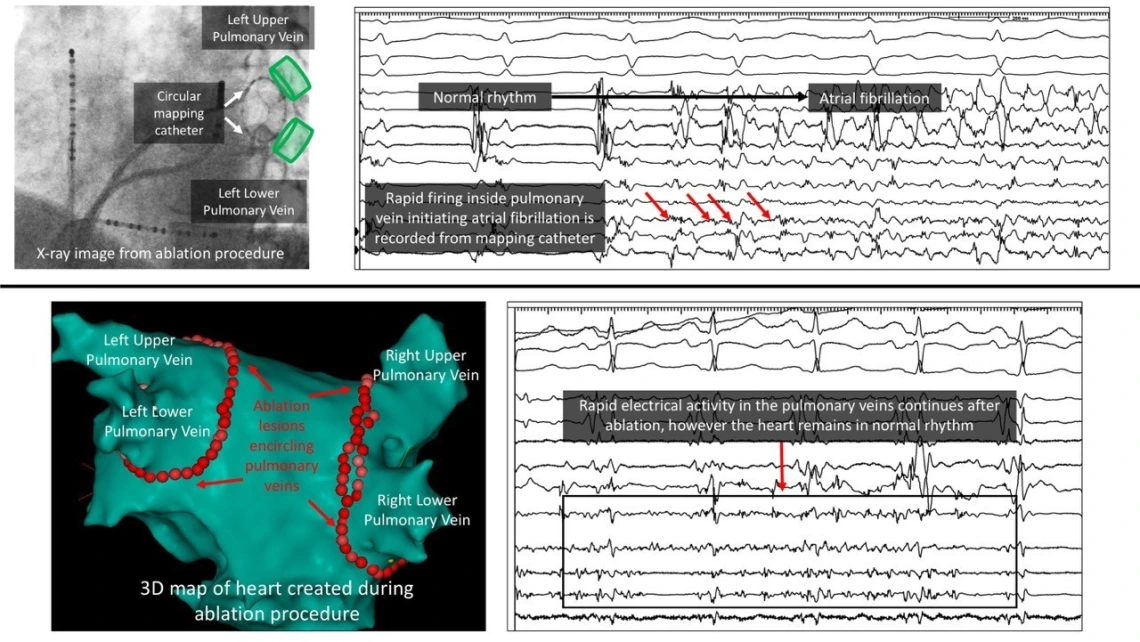
Catheter ablation is a therapy that involves eliminating the regions in the heart that initiate and perpetuate atrial fibrillation. This is done through a heart catheterization (from veins in the groin) and typically requires a single night in the hospital. A variety of different technologies have been developed to improve the safety and effectiveness of the AFib ablation procedure, and patients with intermittent AFib often achieve elimination of their AFib in as much as 80 percent of cases at 1-year post procedure. It is important to have a detailed discussion with your cardiology rhythm specialist to determine whether you qualify for the procedure and which specific approach is best for you.
Left atrial appendage (LAA) closure devices are designed to eliminate the most common source of blood clots that form inside the heart in patients with AFib. These clots can dislodge from the heart and travel to the brain to cause a stroke. LAA closure devices are indicated for people with AFib (not related to a heart valve condition) who have an elevated risk of clotting and bleeding and are not considered long-term candidates for anticoagulation medications (like Coumadin® or warfarin). The decision to proceed with implantation of these devices always is made collaboratively with members of the patient’s care team.
For more information, please visit the UA Sarver Heart Center’s Heart Rhythm webpage and Heart Rhythm Society’s atrial fibrillation page.
Learn More at Oct. 25 Community Lecture
Dr. Hutchinson will present Keeping Your Heart in Sync: What you need to know about atrial fibrillation. This lecture will kick-off the UA Sarver Heart Center’s 30th Anniversary Community Lecture Series. Join us Tuesday, Oct. 25, at 6 p.m. in DuVal Auditorium at Banner – University Medical Center Tucson. Please visit the event page for more information.
About the Author
Mathew Hutchinson, MD, is a professor of medicine at the University of Arizona College of Medicine – Tucson. Dr. Hutchinson is board certified in cardiovascular disease and clinical cardiac electrophysiology, serves as the director of the Cardiac Electrophysiology Program. He specializes in the treatment of complex heart rhythm disorders, such as atrial fibrillation and ventricular tachycardia.

