Connecting with Patricia Lebensohn
Patricia Lebensohn, MD, medical director of the Commitment to Underserved People Program, shared her experiences in a recent issue of The New Physician.
Patricia Lebensohn, MD, originally planned to work as a psychiatrist in her native Argentina before being drawn to family medicine in the U.S.
Family medicine has unique aspects that separate it from other specialties. It is a specialty that treats a broad patient population, thrives on longitudinal care, and serves at the frontline of medicine, often playing a central role in the overall success of the health care system.
Family medicine is characterized by a strong emphasis on preventive therapy, behavioral sciences and a holistic approach to care. The specialty requires a wide range of training in internal medicine, pediatrics, obstetrics and gynecology, psychiatry, and geriatrics. Family medicine physicians transform this knowledge base into a precise discipline, integrating distinct aspects of health to provide comprehensive care.
Like the populations they serve, family medicine physicians are diverse and bring unique personal and professional experiences to the care of their patients. For Patricia Lebensohn, MD, her journey through the medical profession and approach to family medicine is intimately tied to her immigrant journey, her diverse training, and her passion for preventive and integrative medicine.

MD-PhD candidate Andres F. Diaz, MS, wrote this for a recent issue of The New Physician.
Dr. Lebensohn served as the UArizona College of Medicine – Tucson family medicine residency program director from 1999 to 2007. As director, she helped develop the Sports Medicine and the Integrative Family Medicine fellowships. Currently, Dr. Lebensohn serves as director of the Commitment to Underserved People (CUP) Program, an initiative that organizes various student-run community clinics to address health disparities in Tucson and the surrounding region.
Dr. Lebensohn relates her experience in the medical profession, describes the diversity inherent to family medicine, and shares guidance she offers students on the character and qualities required to be a compassionate and competent family medicine physician.
Why did you decide to pursue medicine?
I was born and raised in Rosario, Argentina. In Argentina, students go to medical school right after high school for six years. As you can expect, it is a big decision for a 16 year old to decide then and there to pursue medicine. I originally wanted to pursue a career in art, but I was ultimately drawn to medicine by my father, who was a psychiatrist.
What was your medical school experience like?
I started medical school in 1976, a difficult time in Argentina marked by the military coup that overthrew President Isabel Perón. The timing of my medical education was unfortunate, because at this time it was not safe to be a university student in Argentina. Nonetheless, I finished my education at the age of 22. Medical school in Argentina in the ’70s was much different than what it is now. There were no multiple-choice exams, only oral exams. You really had to know everything!
How did you select your specialty?
I always loved the connection between mind and body. At the time, there was no family medicine residency in Argentina so I decided to pursue psychiatry. I completed my residency in 1987 and soon after moved to the United States with my family. The plan was to stay in the U.S. for a couple of years and then move back to Argentina to work as a psychiatrist. We ultimately ended up staying in the U.S., and I decided to take the board exams for foreign medical graduates.
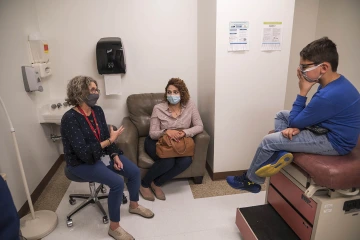
Patricia Lebensohn, MD (left), speaks with a mother and patient in the Shubitz Family Clinic, which is part of the College of Medicine – Tucson’s Commitment to Underserved People program.
It was difficult being an immigrant in the ’80s, especially while taking care of two children. I spoke decent English, which helped, but I had little guidance on how to certify my medical training. I was not sure how to study for my exams — nobody told you how to do so at the time — so I just bought a bunch of question books and read them all. There was no internet in 1987 so books were all we had. Thankfully, I passed all my exams, and once again I had to decide what specialty I wanted to pursue.
At the time, psychiatry was practiced mostly through a biomedical approach, with little emphasis on behavioral sciences. I knew this was not the type of psychiatry I wanted to practice. While I was preparing for my board exams, I worked as a supervisor at a family therapy facility in Syracuse, New York. There, I was first exposed to family medicine and was drawn to its unique approach. These physicians were very involved in different family systems, the biopsychosocial model and the social sciences. After some reflection, I decided to pursue family medicine as a specialty. I applied to the Family Medicine Program at St. Joseph’s Health Center in Syracuse and was accepted in 1990. This was probably the scariest thing I had ever done in my life because I had originally trained in psychiatry and had not been part of any clinical medicine for seven years.
What was your residency experience like?
I was part of an unopposed residency program, meaning that we were the only residents in the hospital at the time. We were the pediatric residents, the NICU (newborn intensive care unit) residents, the OB-GYN (obstetrics and gynecology) residents, the emergency medicine residents — we did it all! I loved my training, despite how rigorous it was. I was able to explore many facets of care and sometimes it felt like I was rotating through various clerkships. I really enjoyed the diversity that family medicine afforded. My training gave me an opportunity to work closely with underserved populations and allowed me to apply my expertise in psychiatry in a more holistic way.
What is a typical day like in your life as a family medicine physician?
There is a large need for family medicine physicians in both clinical settings and academia; the balance of these two worlds really defines my day-to-day work. I always wanted to teach, so my work in academic family medicine is split between teaching medical students and residents and seeing patients in the clinic. My patients are diverse in age, health and socioeconomic status. I work with them to manage chronic disease, maintain health and prevent further illness.
The most common disease or condition I encounter is mental health issues, either as a primary condition or a comorbidity with other conditions. This is why my training in psychiatry became so handy. In combination with family medicine, I can provide holistic psychiatric care that incorporates behavioral science. I also work with the full spectrum of chronic illnesses, including hypertension, diabetes and hyperlipidemia. On the preventive side, I perform physical exams, Pap smears, child wellness checks and many other annual exams. I work closely with nutritionists, behavioral therapists and social workers.
What do you think are essential qualities for success in your specialty?
As a family medicine physician, you have to have a tolerance for ambiguity. You have to acknowledge that you do not know everything. In this specialty you will be a lifelong learner and must be willing to work with others regularly. Also, you have to recognize that you are not going to cure most of the patients you see. Instead, your job is to be there for your patients through their health journey. You are there to improve their quality of life, understand their disabilities and listen to their stories.
To excel in this specialty you have to be able to communicate effectively and cultivate a meaningful physician-patient relationship. This will ultimately foster your training and allow you to become resilient in the face of limited resources or complex social factors that impact your care. Family medicine physicians have a unique attitude about them, one that tells the world, “It does not matter who comes through those doors – I will learn from them, I will help them the best way I can and I will grow with them.
What advice would you give pre-med and medical students or residents about the future of medicine?
I always tell students and residents that they can impact the future of medicine. It does not matter what specialty you pursue; change in medicine can come from many different angles. The main goal is to construct a system that sees health care as a human right and not just a privilege. Everyone should have access to medical care, and this should not be determined by a profit-based business model. You now have the responsibility to think outside of the box and work together to make our health care system a more equitable place for everyone.
A version of this story was originally published by the College of Medicine – Tucson.

