Integrating Indigenous Wisdom and Western Medicine
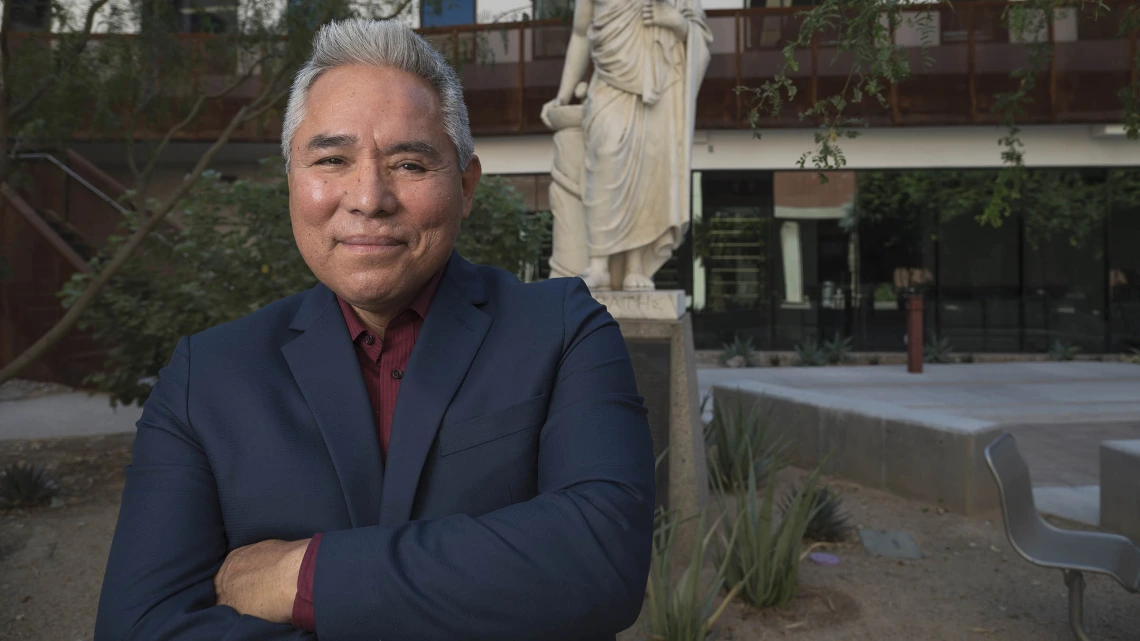
Dr. Tommy Begay is using sleep research to combat PTSD for Native populations impacted by historical trauma.
Tommy K. Begay, PhD, MPH, says environments of toxic stress impact neurophysiology of children, and can lead to unhealthy outcomes as they become adults.
For Tommy K. Begay, PhD, MPH, his work is deeply connected to his and his ancestors’ past.
“The work I do today is based on what I learned from my great-grandmother,” said Dr. Begay. The University of Arizona College of Medicine – Tucson research assistant professor in the Department of Psychiatry and Sleep and Health Research Program studies the neurophysiological impact of adverse childhood stress.
“I currently have an NIH grant (diversity supplement) that's part of the Nogales Cardiometabolic Health and Sleep (NoCHeS) Study,” Dr. Begay said. “The grant provides an opportunity to assess the prevalence of adverse childhood experiences and associated intergenerational trauma in a Mexican-American population along the U.S./Mexico border, and to determine if those factors are linked to poor sleep health and cardiometabolic diseases. This experience also will guide future funding opportunities to further investigate the prevalence of adverse childhood experiences and intergenerational trauma in American Indian/Alaska Native communities.”
Tommy K. Begay, PhD, MPH, in his lab at the College of Medicine – Tucson, says his work today on the impact of childhood stress is connected to the trauma Native people have experienced over the centuries.
“Coming from the Navajo Indian reservation and experiencing the firsthand impact of behaviors associated with interpersonal violence and alcohol abuse, I’ve always been interested in understanding the relationship of American Indian historical trauma and the subsequent evolution of maladaptive coping behaviors currently seen today on reservations and in urban communities,” Dr. Begay said. He said these behavioral outomes are not unique to any particular group, but are experiences seen around the world where there is historical trauma, with outcomes potentially impacting health and behavior.
“Often these maladaptive responses manifest as self-medication, anger, violence and poor sleep, which collectively contribute to negative cognitive, behavioral and health outcomes. All activities and actions lend to physical and functional changes to the brain. These changes influence behavior, subtly becoming embedded into habit, identity and personality.”
“Within Indigenous populations in this country, we see mortality rates for accidents and diabetes mellitus at three times higher than the general population.”Tommy K. Begay, PhD, MPH
Dr. Begay traces the course of historical trauma by pointing to the cultural genocide that resulted from community massacres, genocidal policies, relocation, the prohibition of spiritual and cultural practices, and the forced removal of children from their families into boarding schools. These traumatic experiences have left a legacy of increased prevalence of interpersonal violence, adverse childhood experiences, poor academic achievement and health disparities in this population.
“As a result, within Indigenous populations in this country, we see mortality rates for accidents and diabetes mellitus at three times higher than the general population. Chronic liver disease is five times higher, drug induced deaths are two times higher and suicides are two times higher,” Dr. Begay said.
“We can take those numbers and begin to paint the picture of the effects of maladaptive coping strategies that are associated with adverse childhood stress. This toxic stress has a propensity to change neurodevelopment and impact adult health and wellness.”
Dr. Begay is a cultural psychologist, focusing on the interrelationship of culture, biology and environment to understand human behavior as it applies to health and wellness. He interweaves his Diné/Navajo knowledge and background with Western medicine to improve health outcomes.
As a psychosocial health educator focusing on the “cultures of violence” and primarily working in behavioral health in substance abuse recovery, behavior modification, and in correctional facilities, Dr Begay works with local behavioral health facilities in the Tucson area and at the federal penitentiary, Arizona state prison, Tribal health departments and urban/reservation schools throughout the country.
Studies have linked post-traumatic stress disorder (PTSD) with substance abuse and sleep disorders, such as insomnia and nightmares. Moreover, children with a history of childhood abuse and neglect are at an increased risk of becoming victims of intimate partner violence or becoming a perpetrator of intimate partner violence and childhood abuse.
Dr. Begay said he believes that historical trauma has created a higher risk for intergenerational trauma and cardiometabolic disease in Native American communities.
But resilience – the ability to withstand adversity and bounce back from difficult life events – from Native American cultural and spiritual traditions may provide positive physiological and psychiatric outcomes. Historical trauma decimated the practice of these healing traditions.
Dr. Begay plans to investigate the neurophysiological impact of these healing traditions – especially in regard to sleep health, the body’s natural restorative and healing process.
“My great-grandmother was a traditional Navajo healer; she was a medicine woman; she was an herbalist, collecting medicinal plants. She would talk about this concept that I came to know as natural order. In Diné, this is the foundation of Sa'ah Naghaii Bik'eh Hózhóón, the tradtional Diné worldview and life philosophy,” he said.
“Natural order is just balance. Whatever goes up, has to come down; the sympathetic nervous system goes up, it has to come down. We need to allow it to come down, but in certain places, because of environments of toxic stress, it doesn’t happen for people living in adverse conditions of stress, violence, hunger and poverty. We don't allow the natural healing mechanism of restoration to take place, and this interferes with sleep, and all the good qualities that sleep provides. If people don't sleep, that sets up another trajectory of health outcomes that are related to short sleep (less than 6 hours of sleep).
“These behaviors tend to get moved forward into future generations, since we are primarily social animals, learning from our caregivers, and then from those in our social circles. There are also epigenetic factors that disrupt the formation of genes that code for proteins associated with happiness and wellness.
“We also know that these epigenetic manifestations may be reversed with love, empathy and human connection. Indigenous traditions offer pragmatic approaches to health, wellness and healing. These approaches offer a psychology that focuses on cultural philosophies that integrate the interrelationship of universe, Earth and mind – and the subsequent impact to the body.”
Through this approach, Dr. Begay added, the focus is on calming the nervous system through Indigenous traditional practices, such as talking circles, mindfulness prayer and ceremonial activities like the sweat lodge.
This story was contributed by Jamie Manser, Communication and Marketing Specialist, College of Medicine – Tucson, Department of Psychiatry.

