Dual Pharmacy-Nursing Degree Targets Gaps in Care
Next-generation education at the Colleges of Nursing and Pharmacy aims to fill care gaps as the U.S. physician shortage worsens.

Madison Brandt, RN, is the first Arizona Health Sciences graduate student to pursue a dual Pharmacy-Nursing degree at the University in Arizona and the first recipient of scholarships for the program provided through a $1.4M grant from the Flinn Foundation.
Registered nurse and University of Arizona Health Sciences graduate student Madison Brandt recently pivoted a second time to pursue a career in health care.
First planning to be a physician, Brandt switched her career goal to nursing three years ago as a way to work in health care but in a role that typically involves, in her words, more "one-on-one patient care." And while she loves nursing, it hasn't, on its own, fulfilled her aspirations as a health care professional.
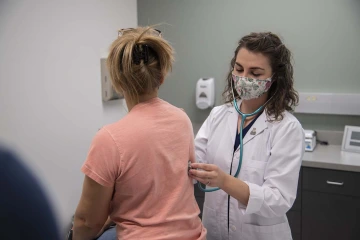
On completing the dual Pharmacy-Nursing degree program, Madison Brandt, already an RN, will have earned an MSN and PharmD, as well as FNP certification.
"I really enjoy the hard sciences like chemistry," Brandt explained. Nursing, she noted, is "much more anatomy and physiology, and so when I saw this dual-degree program, I felt like it blended two things I really love."
The program Brandt refers to launched last year and was recently granted $1.4 million for scholarships from the Arizona-based Flinn Foundation. One of only a few such programs in the country, it combines a master of science degree in nursing, a family nurse practitioner certification and a doctor of pharmacy degree. Graduates earn an impressive alphabet of credentials – MSN, FNP, PharmD – and Brandt is the program’s first student, as well as the first recipient of the newly funded scholarships.
Strategic response
The College of Pharmacy and College of Nursing first proposed the dual degree as a strategy to help answer a growing need in the U.S. health care system, explained Elizabeth Hall-Lipsy, JD, MPH, assistant professor of pharmacy, practice and science, director of the PharmD Forward program and director of the College of Pharmacy Health Disparities Initiative and Community Outreach, who co-led development of the program.

Elizabeth Hall-Lipsy, JD, MPH
And while rural Americans make up about 20% of the U.S. population, their communities are home to fewer than 10% of practicing physicians, making these already underserved areas especially vulnerable to worsening health care gaps.
A vital rural resource
"I work with our rural communities, and staffing is an enormous issue," Hall-Lipsy said, providing an example of a combination clinic/pharmacy. "At all times that pharmacy is open, you need to have a pharmacist working. And any time you want the clinic open, you need a licensed health care provider who has the scope of practice to assess patients, diagnose patients and treat them for any number of circumstances you would expect in someone seeking urgent care."
"For community health centers, rural hospitals, any of those kinds of facilities, a graduate of the dual-degree program will be able to plug in to fill different roles," Hall-Lipsy said. "They're bringing expertise not only in terms of diagnosis and assessment, but also all of their PharmD knowledge about which drug best meets the needs of a patient, works for the formulary at that pharmacy and is safe from potential drug or disease interactions." That person also becomes a key resource for other health professionals in the area, who may have no other direct access to an advanced level of pharmacology training.
Optimizing for existing infrastructure
For patients and health care systems, the advantages of a professional with advanced nursing and pharmacy degrees are many, spanning approachability, effectiveness and accessibility.
Research indicates that nurse practitioners are some of the most effective practitioners today, combining high patient satisfaction scores with fewer medical errors.
Pharmacists, trained to be experts in drugs and individualized medication management, are embedded throughout the U.S. health care system in hospitals, clinics, nursing homes, prisons and – importantly for rural areas – tens of thousands of drug stores, grocers and large discount stores.
At the same time, advanced practice nurse practitioners have expertise in disease prevention, diagnosis and treatment knowledge. Together, the three roles bring prescriptive authority and the skill to deliver hands-on diagnosis and management of common acute and chronic conditions while also being qualified to staff and manage patient care.
Graduating better clinicians
For students, the new dual degree provides the ability to complete in less than six years what otherwise would take at least seven. With any bachelor's degree, they'll enter the College of Nursing Master of Science (MS) in Nursing – Entry to the Profession program, an accelerated (15-month) degree, which is both a pre-licensure and master's generalist program, qualifying graduates to sit for the exam to become a registered nurse.

Terry Badger, PhD, RN
"While they're working as a nurse, gaining experience, students then delve into the first part of their pharmacy studies," explained Terry Badger, PhD, RN, Eleanor Bauwens Endowed Chair, professor of nursing, psychiatry and public health, and chair of the College of Nursing Division of Community and Systems Health Science. "After a year or so, students circle back and finish the family nurse practitioner training, and then they go back into Pharmacy to complete their PharmD."
The structure has the advantage of bringing nursing professional experience to the pharmacy-focused portion of the program, explained Dr. Badger, who co-led planning and implementation of the dual degree. "Because they're actually working with patients who are taking medications as they're completing their degrees, they see how the medications work or don't work and better understand other points of concern."
“We're trying to think forward about what would be the health care needs of the future, and these practitioners will be able to provide a very integrated approach to patient care.”Terry Badger, PhD, RN
"One significant advantage of this approach is that it will help us develop and graduate better clinicians," Dr. Badger continued. "We're trying to think forward about what would be the health care needs of the future, and these practitioners will be able to provide a very integrated approach to patient care."
Health care trailblazer
For Brandt, that more integrated care model is exactly what she hopes to achieve. For anyone interested in becoming a nurse practitioner, she sees the program as offering "a depth of knowledge and a depth of science" beyond that of any standalone advanced nursing degree.
"You'll really have a deep understanding of how the body of your patient is working and the biology behind it," Brand said. "I'm really honored to be kind of the trailblazer of this program. I feel that the University of Arizona Health Sciences really believes in me and believes in making health care more affordable and more accessible."

