Study Uncovers Possible Path for Improving T Cell Therapies
Researchers studied the evolution of the immune system to find a new way to activate T cells to fight infection and disease.
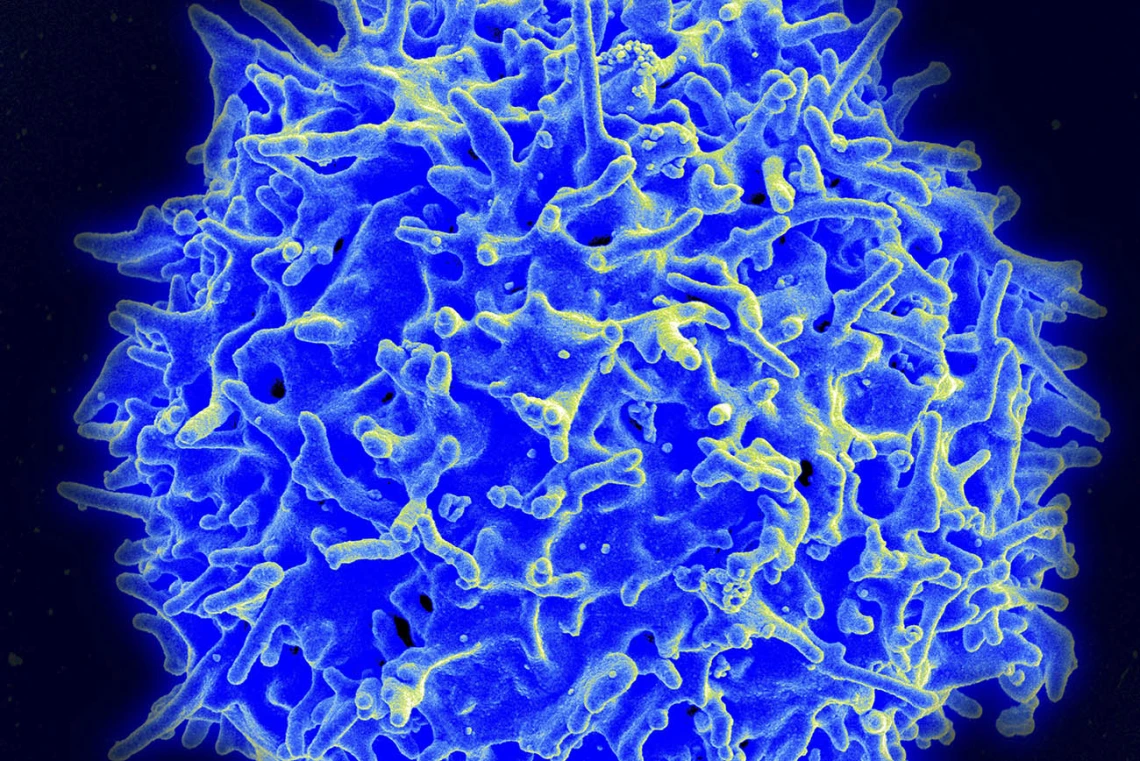
A study led by researchers at the University of Arizona Health Sciences discovered new information about the inner workings of the immune system that could have a profound impact on T cell therapies for cancer and other diseases.

Michael Kuhns, PhD, is an associate professor in the UArizona College of Medicine – Tucson’s Department of Immunobiology.
The study took a unique evolutionary approach to the immune system by examining the ways T cells have changed or remained the same over time. Michael Kuhns, PhD, associate professor in the UArizona College of Medicine – Tucson’s Department of Immunobiology, and Koenraad Van Doorslaer, PhD, assistant professor in the UArizona College of Agriculture and Life Sciences’ School of Animal and Comparative Biomedical Sciences, assembled a team that focused on the evolution and function of CD4.
“This study is giving us a better appreciation for how CD4 works in concert with the T cell receptor to naturally direct T cells,” said Dr. Kuhns who serves on the Center for Advanced Molecular and Immunological Therapies advisory committee. “CD4 is very much a co-equal player in antigen recognition and T cell activation.”
The findings allow researchers to paint a more accurate evolutionary blueprint of the mechanisms within CD4 that could allow for even more powerful versions of T cell therapy. Chimeric antigen receptor (CAR) T cell therapy is already being used for some forms of cancer. Dr. Kuhns and researchers at the Harvard Medical School-affiliated Joslin Diabetes Center, are currently testing genetically engineered five-module CAR T cells as a possible treatment for Type 1 diabetes.
Drs. Kuhns and Van Doorslaer, both members of the BIO5 Institute, looked at CD4 from several different species, from fish to human, to explore more than 400 million years of the molecule’s evolution. They identified regions in CD4 that are unique to mammals.
“We looked at what amino acids in these proteins changed, and what amino acids in these proteins stayed the same,” Dr. Van Doorslaer said. “The idea being, if they didn't change, they could be important for the function of the protein.”

Koenraad Van Doorslaer, PhD, is an assistant professor in the School of Animal and Comparative Biomedical Sciences at the UArizona College of Agriculture and Life Sciences.
“If you think about T cells as being driven by molecular machines, what we do is take the machines apart to figure out how they were built,” Dr. Kuhns said. “CD4 seems to be really important to the function of T cells, because evolution doesn't want it to change. We went in and changed it, which is like looking at how the car works in the absence of the tires.”
More work needs to be done to measure the differing contributions the motifs make to CD4 function. Eventually, the research could lead to the engineering of more finely tuned synthetic receptors for T cell therapies.
The research reported on in this release was supported in part by the National Institute of Allergy and Infectious Diseases (R01AI101053).
Contact
Brian Brennan
Health Sciences Office of Communications
702-604-3088
brianbrennan@arizona.edu

