UA College of Medicine – Phoenix Study Calls for Forensic Nursing Exams to Include Concussion Evaluation
TBIs often missed on routine forensic examination for domestic violence victims.
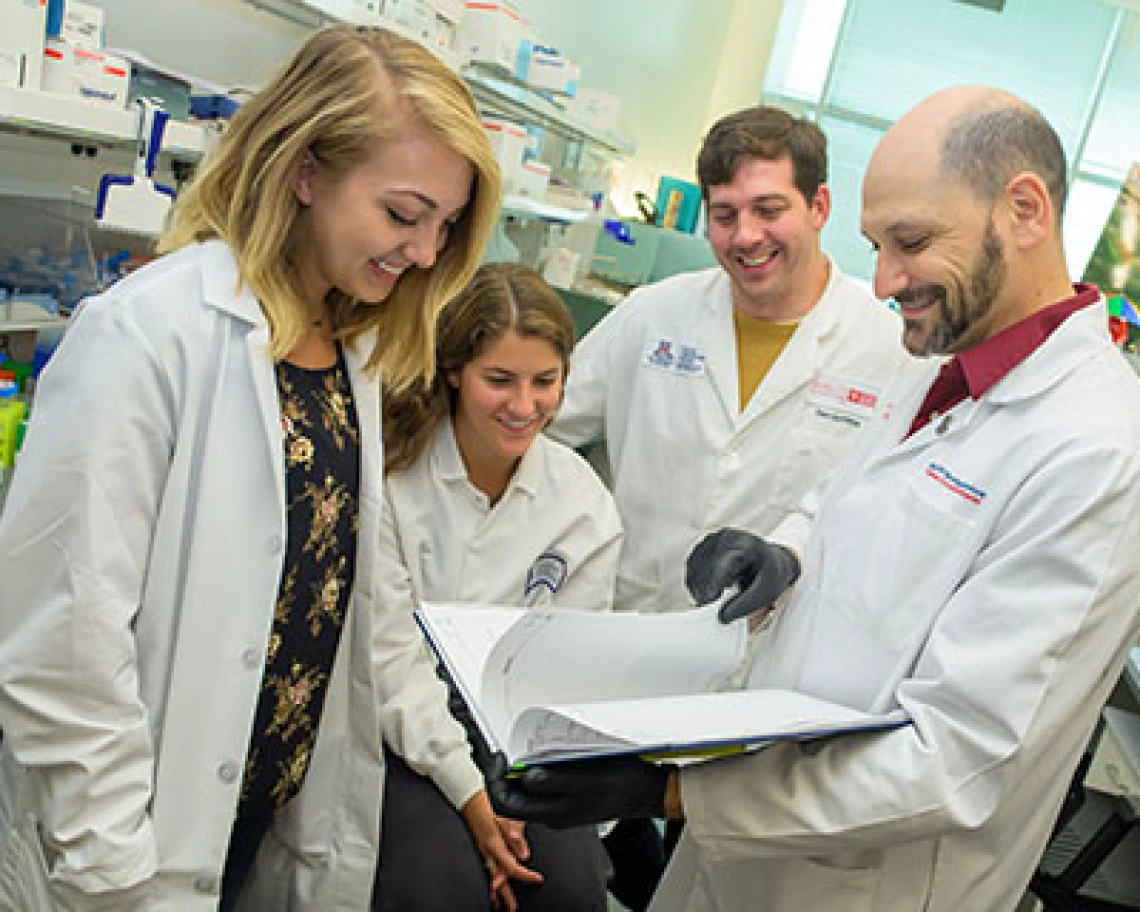
Jonathan Lifshitz, PhD, collaborating with colleagues. Photo by Sun Czar Belous, UA Media Productions.
Intimate partner violence affects an estimated 42 million individuals each year, according to the UA researchers. Multiple research reports estimate as many as 90 percent of these assaults involve physical abuse to the head, neck and face.
“Health-care professionals across disciplines have rarely, if ever, considered domestic violence and intimate partner violence as a cause for TBI,” said Jonathan Lifshitz, PhD, director of the Translational Neurotrauma Research Program at the UA College of Medicine – Phoenix and Barrow Neurological Institute at Phoenix Children’s Hospital. “This arises because in the emergency department other more pressing clinical complaints prevail, like broken bones and lacerations. In the more chronic setting, the victim typically lacks the language or understanding of TBI to articulate the symptoms and need for treatment.”
In the study, which analyzed patient cases from the Mesa Family Advocacy Center between June and July 2017, 100 percent of cases involving strangulation, 52.6 percent of incidents involving a blow to the head with the perpetrator’s hand and 36.8 percent of cases where the victim fell to the ground showed clinical signs of TBI that was undiagnosed during the exam.
“TBI symptoms were evident in all the strangulation cases examined, indicating the likelihood of persistent neurological symptoms that encourage follow-up medical care,” Dr. Lifshitz said.
The study, published in the September issue of the Journal of Aggression, Maltreatment and Trauma, was led by Bridget Ralston, a fourth-year medical student at the college.
Ralston worked with Dr. Lifshitz and Hirsch Handmaker, MD, a research professor of radiology at the medical school and CEO of The CACTIS Foundation, an organization focused on advancing the diagnosis, treatment and prevention of TBIs.
“As a result of these findings, our team proposes an expansion of the exam to include near point of convergence, balance and hand-eye coordination testing to heighten detection of TBI signs in victims,” Dr. Handmaker said. “By detecting these signs early, community efforts can guide patients toward recovery, appropriate treatment options and successful return to society.”
The retrospective review of forensic exams identified data consistent with concussion signs and symptoms. Patient records showed subjective symptoms of dizziness, headache, difficulty breathing, throat pain, cough, loss or change in vision, difficulty swallowing, change in voice, confusion, disorientation and loss of consciousness. Untreated, TBI and concussion can lead to long-term consequences, such as cognitive impairment, suicidal ideation, dementia and early cognitive decline. For patients who show no signs of TBI at an initial examination, symptoms may emerge in a delayed manner and also go untreated. This puts patients at an increased risk for the long-term effects of TBI.
“To continue rigorous forensic exams, our next steps would be to build a database to ‘data mine’ the tens of thousands of existing records and to engage with family-advocacy centers to assign a patient navigator or social worker who can assure equitable access to care,” Dr. Lifshitz said.
DOI: https://www.tandfonline.com/doi/full/10.1080/10926771.2019.1637988
About the UA College of Medicine – Phoenix
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to optimize health and health care in Arizona and beyond. By cultivating collaborative research locally and globally, the college accelerates discovery in a number of critical areas — including cancer, stroke, traumatic brain injury and cardiovascular disease. Championed as a student-centric campus, the college has graduated 500 physicians, all of whom received exceptional training from nine clinical partners and 1,800 diverse faculty members. As the anchor to the Phoenix Biomedical Campus, which is projected to have an economic impact of $3.1 billion by 2025, the college prides itself on engaging with the community, fostering education, inclusion, access and advocacy. For more information, please visit phoenixmed.arizona.edu.
About the University of Arizona Health Sciences
The University of Arizona Health Sciences is the statewide leader in biomedical research and health professions training. The UA Health Sciences includes the UA Colleges of Medicine (Tucson and Phoenix), Nursing, Pharmacy, and the Mel and Enid Zuckerman College of Public Health, with main campus locations in Tucson and the growing Phoenix Biomedical Campus in downtown Phoenix. From these vantage points, the UA Health Sciences reaches across the state of Arizona and the greater Southwest to provide cutting-edge health education, research, patient care and community outreach services. A major economic engine, the UA Health Sciences employs nearly 5,000 people, has approximately 900 faculty members and garners $200 million in research grants and contracts annually. For more information: uahs.arizona.edu (Follow us: Facebook | Twitter | YouTube | LinkedIn | Instagram)

