Creating the future of health care simulation education, training
The Arizona Simulation Technology and Education Center is adapting to the changing health care landscape to train the next generation of providers.

As technology evolves and new health challenges arise, Allan Hamilton, MD, FACS, and the Arizona Simulation Technology and Education Center are developing new ways of educating students, health care professionals, first responders and others.
The future of modern health care simulation and training can be summed up in two words: artificial intelligence.

Allan Hamilton, MD, FACS, is a professor of neurosurgery with additional appointments in radiation oncology, psychology and electrical and computer engineering.
Technological advancements have dramatically changed the way simulation is used to teach and train aspiring health care providers, and AI will be no exception. As AI continues to rapidly evolve and become a part of everyday life, its application in health care simulation will also become commonplace, just as other technologies have become standard in recent years.
“We have more technology available now than ever before. We use augmented reality, mixed reality, immersive reality and high-quality haptics,” said Allan J. Hamilton, MD, FACS, executive director of the University of Arizona Health Sciences Arizona Simulation Technology and Education Center. “There really is this profusion of technology which may, to some extent, improve our educational outcomes. But I look forward to fine-tuning simulation with AI.”
Health care simulation is a range of activities that share a broad, similar purpose – to improve the safety, effectiveness and efficiency of health care services.
Dr. Hamilton recently discussed how health care simulation has evolved, how AI can best be implemented and what is next for simulation in educating the next generation of health care professionals.
Q: How has simulation changed in recent years?
Dr. Hamilton: When medical simulation started to take off about 20 years ago, for a long time it was a little bit like the Wild West because all the equipment was different and everybody’s approach was different. As the field consolidated, the theme of using it in education and training became more dominant. The fact that it was immersive really drove it to where it is today. The patient’s experience in health care settings is different now than it used to be, which means the opportunities to train students have changed, too. It used to be, as a physician, I might see a patient in clinic, then I might see them in the operating room if they are having a procedure and I would see them post-operation. Now it is completely different. A patient will go into a hospital and see a pre-ops team, then a completely different team does the surgery, then there’s a post-ops team that handles you before being discharged. So that delegation has completely broken up the patient’s experience.
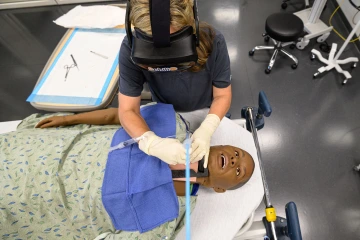
ASTEC can test new technologies, such as 8Chili's HintVR™ headset, to determine the best way to integrate them into educational programs.
Dr. Hamilton: From an education and training perspective, it is hard now for one of our students to be able to intercept and see everything from start to finish for a particular patient. That is where medical simulation is really a strength because we can go back and teach what may have been missed in the clinical experience for a student. If a student didn’t see a heart attack case when they were in the unit, we can simulate one. So, in a sense it has evolved to a point where it allows us to standardize things and consider problems of patient continuity. For us at ASTEC, our education gets divided into procedural-based training, scenario-based training, and then interprofessional education and leadership.
Q: What role can AI have for medical training?
Dr. Hamilton: I am really looking forward to fine-tuning simulation with AI. I would like for everybody to have an AI coach that says ‘I am with you throughout your education and training, and throughout your career as a health care provider’. An AI coach could provide personal feedback of what a student is doing well, what they need to do better. It can look at how they are doing on procedures and how they are doing on patient interviews. It can identify if one institution is having problems with certain kinds of infections while others are not. So, the idea is to have this telling you at every step of the way what to work on and simulate so that you are going to do better and make you the absolute best practitioner the world has ever seen.
Q: Can medical simulation and the introduction of AI help develop leaders?
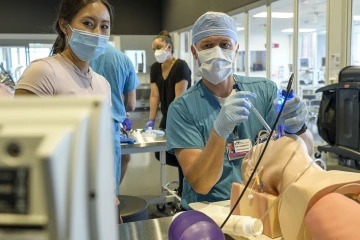
Medical simulation can be designed to meet the specific needs of the users, such as the Department of Anesthesiology utilizing ASTEC for a training session. Dr. Hamilton notes that there are subtle differences in the needs of training anesthesiologists versus anesthetists, and that ASTEC consults with experts in all specialties to ensure all needs are met.
Dr. Hamilton: First, I would say that none of us are leaders all the time. I may be very good in the operating room, but lousy with prevention. But there are a couple ways that simulation helps build leadership. One way is with culture, which is you can use these exercises and programs to reinforce the values that you want in your medical professionals. For instance, your values could be: be respectful, communicate well and acknowledge the effort of other people on your team. That’s where AI can really help us, too. Is a student good at performing their tasks, but they aren’t good at noticing or helping when others may have a problem and need help? An AI coach could step in and say, “You need to be better as a team member and here are some tools to practice that.” In the past, that was up to the capriciousness of human beings. One student might have a great coach or mentor, but another might have a terrible mentor. With AI, we might be able to be more effective at teaching because we will be more consistent at developing medical professionals who are more readily prepared to work with one another once they interact in the clinic.
Q: What lies ahead for medical simulation?
Dr. Hamilton: The answer is more. Every single problem that we've had in medicine is only getting worse. Shortages of personnel are continuing, patients are being moved through the system faster and faster to maximize profitability, and there is much more outpatient care than we ever had before. The breakup of continuity in patient care doesn’t provide enough range for us to teach students. Back when I was training, I might see 100 cases of certain types of patients. Now, they might not see any, or only a couple, of a certain patient. Medical simulation allows us to create those patients and those scenarios.

Students in the nurse-midwifery program, led by Erin McMahon, EdD, CNM, FACNM (center), get hands-on experience through clinical simulations at ASTEC.
The last part of this is that the processes we can simulate allow for the patient to have the absolute safest experience. Our goal at ASTEC is to look toward a world in which no one suffers an avoidable medical adverse event. That’s our goal, and in order to achieve that, we have to stay at the top of our game now and in the future.
Our Experts
Allan J. Hamilton, MD, FACS
Executive Director, ASTEC
Clinical Professor, Radiation Oncology
Professor, Surgery
Professor, Psychology
Professor, Electrical and Computer Engineering
Contact
Blair Willis
Health Sciences Office of Communications
520-419-2979
bmw23@arizona.edu

