Respiratory Tract Bacterial Extracts Could Prevent COVID-19, Study Finds
Bacterial lysate OM-85 blocked SARS-CoV-2 infection by decreasing the coronavirus's ability to bind to the lung cell surface receptor ACE2, research found.
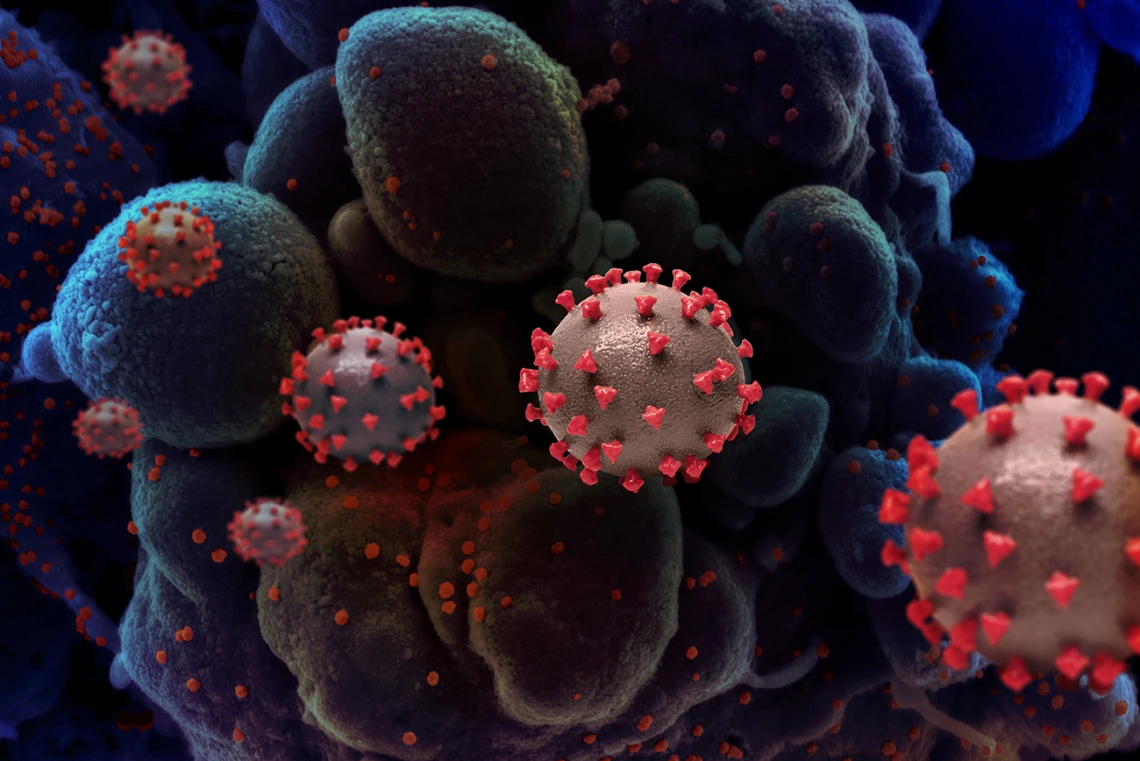
UArizona Health Sciences researchers are targeting the ACE2 receptor, using bacterial extracts to close the door that allows the SARS-CoV-2 virus to infect cells. (Credit: National Institute of Allergy and Infectious Diseases, NIH)
A team of University of Arizona Health Sciences researchers at the UArizona College of Medicine – Tucson found that a combination of bacterial extracts used in Europe to treat respiratory infections may offer a new way to prevent or reduce infection by SARS-CoV-2, the virus that causes COVID-19.

Donata Vercelli, MD, is a professor of cellular and molecular medicine at the UArizona College of Medicine – Tucson and of genetics at the BIO5 Institute.
“Current infection prevention strategies rely on vaccines that trigger our immune system to respond primarily by producing antibodies. The antibodies attach to a specific part of the virus that acts like the key and prevent it from being able to attach to the lung cell receptor, which is like a lock on the outside of the lung cell. This study is unique because it is the first time researchers have targeted the receptor – the lock – with a bacterial extract and shown it protects against infection with live virus. We’re essentially removing the lock from the cell wall so there’s nothing for the virus’ key to attach to,” said senior author Donata Vercelli, MD, professor of cellular and molecular medicine at the UArizona College of Medicine – Tucson and of genetics at the BIO5 Institute.
When SARS-CoV-2 enters the lungs, it binds to receptors including the angiotensin converting enzyme 2 (ACE2) receptor on the outer membranes of lung cells. A cellular enzyme changes the shape of a protein on the virus to enable SARS-CoV-2 to breach the membrane and infect the cell.
When the pandemic began, Dr. Vercelli, Vadim Pivniouk, PhD, associate professor in the College of Medicine – Tucson’s Department of Cellular and Molecular Medicine, and other members of the research team turned to data they collected in an asthma prevention study to determine whether OM-85 treatment affected the ACE2 receptor and enzyme involved in COVID-19.
Dr. Vercelli collaborated with Janko Nikolich-Žugich, MD, PhD, professor and chair of the College of Medicine – Tucson’s Department of Immunobiology and BIO5 member, and Jennifer Uhrlaub, associate research scientist, and found that pretreatment of cells with OM-85 prevented infection by SARS-CoV-2. The ability of OM-85 to prevent viral infection was found to be dependent on its ability to decrease the expression of the ACE2 receptor.
“ACE2 is the critical piece that tips the scale,” said Dr. Vercelli, who also serves as director for molecular genomics at the Asthma and Airway Disease Research Center. “Without that initial attachment – the key fitting into a lock – the entire infectious process is derailed and blocked.”
The mechanism by which OM-85 prevents viral infection is unlike that of vaccines or antibody treatments, which focus on a viral protein. By targeting the receptor, OM-85 may shut the very door that allows the coronavirus to infect cells, which could make it effective against any variants that infect cells through the ACE2 receptor.
“Original studies of this type require us to test whether infection by the live virus can be blocked by the potential preventive treatment in question,” Dr. Nikolich-Žugich said. “This must be done in specialized biosafety containment facilities, so our long-time experience with this type of work and our biosafety facility at BIO5 enabled us to help Dr. Vercelli and her team with this study.”
Drs. Vercelli and Pivniouk also enlisted the help of Monica Kraft, MD, the Robert and Irene Flinn Endowed Chair in the College of Medicine – Tucson, who collected primary lung cells from healthy patients.
The rationale for using bacterial extracts to prevent viral infection relates to a previous study led by Dr. Vercelli, who also is the director of the Arizona Center for the Biology of Complex Diseases. In 2016, her team found that exposure to environmental microbial products protected Amish farm children from asthma and allergies.
“Our innate immune system has evolved under environmental pressures like bacteria, but our current lifestyles often don’t give us the chance to develop this protective immunity,” Dr. Vercelli said. “Our idea is to use bacterial lysate to train our immune system to protect us from viruses, in the same way those who are regularly exposed to farm animals are protected against a multitude of bacteria and other microbes.”
According to Dr. Vercelli, treatment with bacterial lysates such as OM-85 could promote a more interactive exchange between the immune system and microbes.
This research was supported in part by OM Pharma SA, and by the National Institutes of Health’s National Institute of Environmental Health Sciences (T32ES007091), National Heart, Lung and Blood Institute (T32 HL007249, R25HL126140), and National Institute of Allergy and Infectious Diseases (P01AI148104, R21AI144722).

