UArizona Health Sciences Researchers Add Clarity to Role of Blood Pressure Medications in COVID-19 Infections
Sarver Heart Center researchers clarify the interaction between blood pressure medications and SARS-CoV-2, the virus that causes COVID-19.

Researchers find blood pressure medications do not increase the likelihood of SARS-CoV-2 infection, good news for people with hypertension, or uncontrolled high blood pressure.
A study led by researchers in the Sarver Heart Center at the University of Arizona College of Medicine – Tucson addressed concerns about the use of blood pressure medications and patients’ susceptibility to infection of SARS-CoV-2, the virus that causes COVID-19. They found that blood pressure medications do not increase the likelihood of SARS-CoV-2 infection, which is good news for people with hypertension, or uncontrolled high blood pressure.

First author Jessika Iwanski, a dual MD/PhD candidate, led the translational research team.
“Throughout the pandemic, we have recommended that people continue to take their prescribed antihypertensive drugs. This is critical to reducing heart disease events, especially since people with heart disease are more susceptible to severe COVID-19 complications,” said Nancy K. Sweitzer, MD, PhD, professor of medicine and director of the UArizona Sarver Heart Center, who was not involved in the study. “The study is very reassuring to clinicians who prescribe these drugs to patients regularly, as it adds important evidence that they do not worsen SARS-CoV-2 infection.”
The paper, “Antihypertensive drug treatment and susceptibility to SARS-CoV-2 infection in human PSC-derived cardiomyocytes and primary endothelial cells,” was published in Stem Cell Reports.
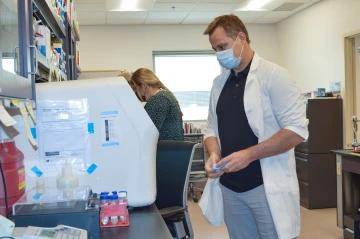
Jared Churko, PhD, assistant professor of cellular and molecular medicine in the College of Medicine – Tucson and director of the University of Arizona induced Pluripotent Stem Cell (iPSC) Core, used stem cells to evaluate the impact of blood pressure medications on SARS-CoV-2.
Jared Churko, PhD, assistant professor of cellular and molecular medicine in the College of Medicine – Tucson and director of the University of Arizona induced Pluripotent Stem Cell (iPSC) Core, used stem cells to evaluate the impact of blood pressure medications on SARS-CoV-2. Stem cells are cells that have the potential to become any cell type in the body. In this study, the research team generated heart cells (cardiomyocytes) from human pluripotent stem cells and primary endothelial cells using discarded tissue from consenting open-heart surgery patients.
Both cell types were then infected with SARS-CoV-2, and significant changes in genes involved in inflammation and cell function were observed. However, the presence of blood pressure medications, such as losartan or lisinopril, did not alter the levels of SARS-CoV-2 entering the cells.
“These findings demonstrate that SARS-CoV-2 can be harmful to cardiomyocytes,” Dr. Churko said. “Together with data from large trials of patients prescribed ACEIs and ARBs, the findings also suggest that treatment with blood pressure medications does not alter SARS-CoV-2 infection at the cellular level.”
“These classes of medications are used in many other conditions as well, including diabetes, kidney disease and heart failure because, in addition to lowering blood pressure, they can reduce deposition of scar tissue in organs, and reduce abnormal signaling in cells and organs that contribute to abnormal growth and enlargement,” Dr. Sweitzer added. “They have also been shown to be particularly effective in reducing heart disease events in patients with diabetes who also have even mild elevations in blood pressure.”
Hypertension is a significant cause of heart disease, the leading cause of death in the United States. The Centers for Disease Control and Prevention estimates that 116 million adults in the U.S. have high blood pressure. While first line treatment includes recommendations for lifestyle changes, most adults ultimately need medications to control high blood pressure.
The translational research team was led by first author Jessika Iwanski, a dual MD/PhD candidate in the laboratory of co-author Carol Gregorio, PhD. The team also included scientists and physicians from UArizona College of Medicine – Tucson, BIO5 Institute and Sarver Heart Center.
This research was supported in part by a UArizona Sarver Heart Center Investigator Award, funded by the Steven M. Gootter Foundation, and by the National Heart, Lung and Blood Institute of the National Institutes of Health (R00HL128906, F30HL151139, T32HL007249).
Contact
Katie Maass
520-626-4083
KMaass@SHC.Arizona.edu

