Stimulating the brain to treat pain and substance use disorder
Comprehensive Center for Pain and Addiction researchers are studying how electronic stimulation of the brain can break looping pain signals and destructive cravings.
For a person with chronic pain or a mental health condition, the phrase “it’s all in your head” can be a particularly frustrating expression. While they are experiencing something very real within the body, there is truth behind the sentiment that the brain controls our perceptions.
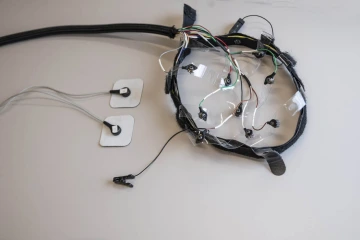
A wearable device from the company Ni2o is being used to study transcranial direct current stimulation for the treatment of chronic pain and substance use disorder.
University of Arizona Health Sciences researchers are asking the question: if the brain plays a primary role in how we think and feel, could therapies be designed to target the brain and improve certain conditions? One therapy, transcranial direct current stimulation, or tDCS, uses electronic pulses to stimulate areas of the brain. Participants are currently being recruited for two studies measuring how tDCS can be used to treat chronic pain and substance use disorder.
“Historically, treatments for these conditions have taken a one-size-fits-all approach. For chronic pain, patients often receive medications that can lead to dependence. For substance use disorder, patients go into some form of cognitive behavioral therapy, but the chance of recurrence rate in using a substance is high,” said Allison J. Huff, DHEd, assistant professor in the Department of Family and Community Medicine at the UArizona College of Medicine – Tucson. “I am excited to find a more precise treatment and to give power back to the patient.”
Dr. Huff and her mentor Todd Vanderah, PhD, director of the Comprehensive Center for Pain and Addiction and head of the Department of Pharmacology at the College of Medicine – Tucson, are using similar protocols for both studies. One looks at participants who have chronic pain and the other examines those with substance use disorder.
“You can think of chronic pain and substance use disorder as a kind of loop happening in the brain, similar to how intrusive thoughts loop over and over again in anxiety or obsessive-compulsive disorder,” Dr. Vanderah said. “We know that the brain can get stuck in a pattern that can exacerbate pain signals. We hope that tDCS treatment will help break that loop when it comes to chronic pain and the impulse to use drugs.”
Stopping the pattern of pain

Allison J. Huff, DHEd, focuses much of her research on the impact of acculturation and sociocultural factors of substance use and abuse.
Transcranial direct current stimulation has been shown to have a therapeutic effect on neurodegenerative diseases such as Parkinson’s and Alzheimer’s. It works by stimulating the prefrontal cortex region of the brain, where decision making occurs. The prefrontal cortex is essential to reasoning, problem solving and impulse control.
In both studies, Drs. Huff and Vanderah partnered with the company ni2o, which provided a wearable device that can deliver subtle yet stimulating zaps to the prefrontal cortex. Participants receive seven tDCS treatments over 11 days. Their brainwaves will be monitored during each visit to see at what dosage and frequency a change occurs.
“Neurotransmitters like serotonin, dopamine and adrenaline play important roles in the nervous system and the brain. They also have a lot to do with how we perceive pain,” Dr. Huff said. “There is evidence tDCS can impact these neurotransmitters.”
Many people have heard stories of how someone might withstand tremendous amounts of pain when a neurotransmitter such as adrenaline is surging through their veins. But while the brain has the ability to suppress pain, it can also enhance it, Dr. Vanderah said. In people with chronic pain, the prefrontal cortex may be fixating on the pain and stuck in a feedback loop that won’t turn off.

Todd Vanderah, PhD, has focused on finding ways to manage pain without increasing the risk of addiction.
“While tDCS will not shut off these pain signals, it may be able to break the loop and change the way the brain is enhancing the pain signal,” Dr. Vanderah said.
The relationship between the mind and body when it comes to pain is something most people have probably experienced in their day-to-day lives.
“You might have noticed your pain tolerance can change depending on your mood, if you know the pain is only temporary, or even what day of the week it is,” Dr. Huff said. “All these things can impact how much you feel the pain.”
Shutting off the cravings of addiction
The prefrontal cortex also plays an important role in impulse control, which is often in direct conflict with another portion of the brain known as the limbic system. The limbic system deals in functions primarily associated with survival and is sometimes referred to as the “animal brain.” Humans' large prefrontal cortex often overrides the limbic system’s drive for immediate gratification in favor of long-term goals.
“You don’t see animals doing crazy things like going to school for many years to get a degree in the hopes to land a good job one day,” Dr. Vanderah said jokingly. “It is the prefrontal cortex that helps us decide to stick to a plan, even if there is a short-term cost, when it might pay off down the road.”
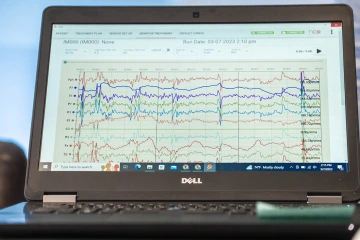
Participants’ brain waves are monitored by an electroencephalogram, or EEG. Electrical activity in the brain shows up as wavy lines on an EEG recording.
Dr. Vanderah also uses the example of ice cream. While the limbic system might desire 10 scoops of ice cream, the prefrontal cortex might help make the decision to eat a more reasonable amount. In the case of substance use disorder, the prefrontal cortex may be wired to lose that battle.
“Many of us have had people in our lives who make us wonder how they can make the decisions they make. If you talk to someone with substance use disorder when they are sober, they will often tell you they knew they were making the wrong decision,” Dr. Vanderah said. “In this case, the limbic system may be overriding the prefrontal cortex.”
Stimulating the prefrontal cortex with tDCS could help treat substance use disorder by giving it a boost against the impulsive cravings coming from the limbic system.
Dr. Huff said the two studies will provide information that could eventually lead to more precise treatments for chronic pain and substance use disorder. Future clinical trials could tailor tDCS treatments to the individual by using their observations to adjust the dosage and frequency to the optimum level for each patient.
“It is amazing how chronic pain and substance use disorder are two different things, but they share so many similarities when you look at them in relation to the brain,” Dr. Huff said. “These patients often know their disorder or disease better than anyone. They know their triggers, and they know what helps them. tDCS is a tool that might help empower their own management of these conditions.”
Our Experts
Allison J. Huff, DHEd
Assistant Professor, Department of Family and Community Medicine, College of Medicine – Tucson
Todd Vanderah, PhD
Professor and Head, Department of Pharmacology, College of Medicine – Tucson
Director, Comprehensive Center for Pain and Addiction
Co-Director, MD/PhD Dual Degree Program
Professor, Anesthesiology
Professor, Neurology
Member, BIO5 Institute
Member, Cancer Biology Program, UArizona Cancer Center
Contact
Brian Brennan
Health Sciences Office of Communications
520-621-3510
brianbrennan@arizona.edu

