Applying A Team Approach to Health Care Education
Interprofessional education modules at the Arizona Simulation Technology and Education Center teach students the importance of teamwork in health care.

The Arizona Simulation Technology and Education Center is piloting a series of games and clinical exercises that challenge small interdisciplinary groups of University of Arizona Health Sciences students to accomplish tasks as a team.
Hannah Rosen stood with her feet together and looked to her left, then to her right. Should she step forward? Or maybe take one step back? She knew a wrong step could be her last.
“Go with your gut!” an authoritative voice implored.
Rosen, an undergraduate student at the University of Arizona Health Sciences, thought carefully for another moment before deciding out loud, “I’m going to step on it.”
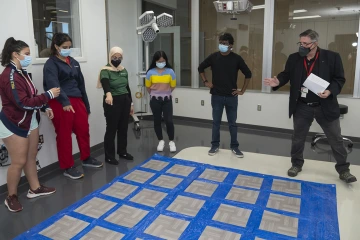
(From left to right): Hannah Rosen, Nadja Jones, Diyana Ahmad, Lyr Cerilla and Aryan Eksambe listen to Allan J. Hamilton, MD, FACS, explain the basic concepts and rules of the "Toxic Tile" game.
As Rosen stepped forward safely, she exhaled with relief. Her four teammates, watching anxiously on the side, let out a collective laugh. Rosen smiled with them, but only for a brief moment. She had another step to take.
Five students faced the same trial-and-error decisions as they attempted to conquer the “Toxic Tile” game. Set up in a 5-by-7 grid of tiles, the game challenged the students to figure out a sequence of “safe” steps, one tile at a time, to reach the other side. A wrong step was “toxic,” and the student who took that misstep went to the back of the line.
The only person with the code to successfully cross the toxic maze was Allan J. Hamilton, MD, FACS, executive director of the Arizona Simulation Technology and Education Center (ASTEC) at UArizona Health Sciences. It was his voice that occasionally offered encouragement, but otherwise he let the students solve the maze by learning from each other’s missteps.
“Team skills have been identified as an area that need significant improvement in medicine,” said Dr. Hamilton, a Regents Professor of Neurosurgery in the College of Medicine-Tucson. “The tile game was meant to build up team skills and see how the students could work together.”
The tile game is one of many interprofessional education (IPE) games, or small team modules, ASTEC offers to foster teamwork among students from different Health Sciences’ colleges.
“We created a series of small-team modules for students from different disciplines,” Dr. Hamilton said. “We put them in situations that require them to work as a team. We aren’t focused specifically on their clinical skills; we want to see what they can do as members of a team.”
Education for a changing field
An already evolving health care landscape was further changed by the COVID-19 pandemic, which forced hospitals to split staffing to protect health care providers from all being sidelined by COVID-19 at the same time. It also eliminated many face-to-face interactions between patients and providers. The need for a team-based approach to medicine became clearer than ever.

Dr. Hamilton believes interprofessional education activities are essential for today’s aspiring health professional because he says that team skills are more important than ever in order to be a successful health care provider.
“There used to be an old idea that as a doctor, you are the captain of your ship and you run everything and give the orders,” Dr. Hamilton explained. “That doesn’t hold up anymore. COVID was humbling in terms of teaching us that without a team, it was impossible to do what we needed to do.”
As health care professionals adapted to new patient care models, a new need arose – students must be educated and trained to become adept at working in interdisciplinary teams. ASTEC offered the ideal environment to launch new IPE modules.
“We are here to get people out of their silos,” Dr. Hamilton said of the ASTEC team that includes David Biffar, MS, CHSOS- A, director of operations, as well as a host of research, simulation and education specialists. “If there is a constant theme across what we do, it is the idea that we are going to do things that are interdisciplinary. It’s not just medicine or just nursing, it’s everyone in the Health Sciences.”
The IPE learning groups typically include five to eight students from at least two of the five Health Sciences colleges – the College of Medicine – Tucson, College of Medicine – Phoenix, College of Nursing, R. Ken Coit College of Pharmacy and Mel and Enid Zuckerman College of Public Health. The IPE groups are one of the ways in which ASTEC brings students – and their unique areas of expertise – together. Doing so gives the students the opportunity to learn things that might not be in their textbooks.
IPE exercises can also be a fun. After completing the tile game, Rosen and her teammates – one from the Coit College of Pharmacy, one from the College of Medicine – Tucson and two fellow pre-med students – enjoyed pizza and conversation with one another.
When Dr. Hamilton asked them how they felt, “accomplished” was their first response.
Simulating real-world scenarios
Many of the IPE modules that Dr. Hamilton leads, such as the tile game, are designed to build team skills in general. Others have more realistic scenarios and are based on actual experiences.
“We are here to get people out of their silos.”
Allan J. Hamilton, MD, FACS
When Dr. Hamilton was working in a Boston hospital more than three decades ago, a fire broke out. Emergency personnel responding to the fire call quickly began ordering everyone to evacuate.
For years, Dr. Hamilton has simulated that scenario, smoke included, with students. He is especially interested in how the students respond when the smoke emerges, fire alarms are blaring and orders to evacuate are being shouted out.
“In emergencies, you must think quickly and clearly. To do that, you have to be calm and you have to be able to work together,” Dr. Hamilton said. “For instance, I can’t evacuate and expect that my patients are going to be okay and that my team will handle everything. I have to use my judgement to know what is best and what my responsibilities are.”
Deana Smith, BSBA, BSN, RN, also has experience in a hospital fire. Her nursing background is especially helpful in leading ASTEC’s clinically based IPE modules, which include events focused on rescuing drowning victims and mass-casualty scenarios.
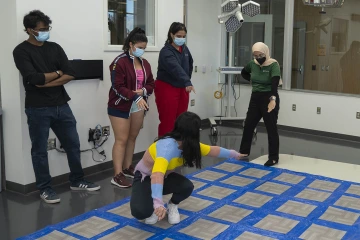
To successfully navigate the grid of “toxic” tiles, students had to learn from the missteps of those who went before them by identifying patterns and sequences of safe steps.
“I like to give our learners something they can use, especially if they haven’t been a part of the hospital system yet,” Smith said.
Smith also leads IPE modules focused on diversity and inclusion in health care. She was recently recognized by the Office of Equity, Diversity and Inclusion at the UArizona Health Sciences LGBTQIA+ Community Networking and Pride Awards.
“It’s important to ensure our IPEs are inclusive so our learners understand how to interact with all people in the clinical setting,” Smith said. “For instance, how do we interview a transgender person? What are some of things we should avoid saying? What are the relevant health issues we need to be addressing?”
A model for the future
ASTEC hosted 16 IPE modules during the fall semester. After each one, participants were asked to complete a five-pronged assessment. Dr. Hamilton says the sessions have scored highly among the students, who don’t earn any course credits for the experience.
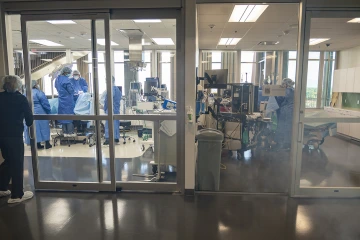
An IPE module simulated a scenario where smoke appears next door to an operating room. The participants were alerted to the smoke and instructed to evacuate.
Dr. Hamilton hopes to change that. He plans to continue piloting the IPEs and collecting data that could be presented to leadership across the Health Sciences, including the deans of the colleges.
“These students are volunteering for these sessions on their own time,” Dr. Hamilton said. “They have a full course load, so in a way this is extracurricular. They’re using their lunch break or their weekends to do these IPEs. Once we have the data, we hope to be able to show the colleges that they should make more time for students to officially participate in these activities.”
Dr. Hamilton believes the addition of specialty degree programs for nurse-midwifery, physician assistant and physical therapy programs are the latest reminder of how imperative interprofessional education will become in the future.
“We will be in the team business, learning and training alongside each other,” he said. “Hopefully what we are piloting now will be front and center down the road.”
Our Experts
Allan J. Hamilton, MD, FACS
Executive Director, ASTEC
Clinical Professor, Radiation Oncology
Professor, Surgery
Professor, Psychology
Professor, Electrical and Computer Engineering
Deana Smith, BSBA, BSN, RN
Educator, Healthcare Simulation
David Biffar, MS, CHSOS- A
Director of Operations
Contact
Blair Willis
Health Sciences Office of Communications
520-419-2979
bmw23@arizona.edu

